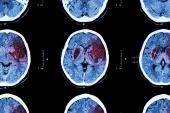
LASTE Shows Thrombectomy Helps for Large Strokes of All Sizes
Despite an increase in hemorrhage and some complications, the net benefit clearly favors thrombectomy, one expert says.

Extending the results of several prior trials of thrombectomy in patients with large-core acute ischemic strokes, LASTE demonstrates that the intervention remains beneficial even when there is no cap on the size of the infarct.
Among patients with an Alberta Stroke Program Early Computed Tomographic Score (ASPECTS) of 5 or lower, with no bottom limit, thrombectomy plus medical care improved the likelihood of a better functional outcome at 90 days compared with medical care alone (generalized OR 1.63; 95% CI 1.29-2.06), report researchers led by Vincent Costalat, MD, PhD (Hopital Gui de Chauliac, Montpellier, France) and Tudor Jovin, MD (Cooper Neurological Institute and Cooper Medical School of Rowan University, Camden, NJ).
“This finding,” they write in the May 9, 2024, issue of the New England Journal of Medicine, “corresponds to a number needed to treat of 4 (95% CI 3 to 8) for one patient to have a decreased modified Rankin Scale score at 90 days with thrombectomy plus medical care as compared with medical care alone.”
The intervention also lowered the rate of all-cause death over the same span (36.1% vs 55.5%; (adjusted RR 0.65; 95% CI 0.50-0.84). Those benefits came at the cost of a higher rate of symptomatic intracerebral hemorrhage and 11 procedure-related complications in the thrombectomy arm.
Commenting for TCTMD, Götz Thomalla, MD (University Hospital Hamburg-Eppendorf, Germany), noted that what sets LASTE apart from prior thrombectomy trials in patients with large-core strokes—including RESCUE-Japan LIMIT, SELECT2, and ANGEL-ASPECT—is that there was no lower ASPECTS limit for inclusion; those prior trials mostly included patients with ASPECTS of 3 to 5.
Importantly, Thomalla said, a subgroup analysis in LASTE showed no variation in the treatment effect between patients with an ASPECTS of 2 or lower and those with an ASPECTS of 3 or higher. He added that most prior thrombectomy trials have not shown a mortality advantage for thrombectomy either.
Overall, the LASTE results are reassuring when it comes to the efficacy and safety of thrombectomy in patients with even larger infarcts (ie, lower ASPECTS) than previously studied. “The net benefit is clearly there,” Thomalla stressed.
The LASTE Trial
LASTE, conducted in 24 high-volume stroke centers experienced in thrombectomy in France and six in Spain, included 324 patients (median age 74 years; 52% men) who presented within 6.5 hours after symptom onset with a proximal cerebral vessel occlusion in the anterior circulation and a large infarct defined by an ASPECTS of 5 or lower detected by MRI or CT (for patients older than 80, it had to be 4 or 5). The trial was stopped early in February 2023 after the positive results of the other large-core trials raised questions about whether it would be ethical to continue.
In LASTE, the median ASPECTS was 2, with more than half of patients (56%) having a score of 2 or lower. The median time from symptom onset to randomization was about 4.5 hours, and about 35% of patients in both groups were treated with thrombolysis. Use of IV thrombolytics and other medications was left to the discretion of the treating physicians.
The primary outcome was the score on the modified Rankin Scale (mRS) at 90 days—the median score was 4 in the thrombectomy arm and 6 in the medical-care arm, a significant advantage for the procedure. This difference was maintained out to 6 months.
Thrombectomy also significantly improved quality of life at 90 and 180 days, lowered the rate of decompressive craniectomy within 7 days (8.8% vs 11.5%), and increased the rate of early neurologic improvement (30.7% vs 11.4%). Moreover, the mean change in infarct volume between baseline and 24 hours was smaller with thrombectomy versus medical care alone (51.6 vs 119.5 mL).
On the safety side, thrombectomy increased the rate of symptomatic intracerebral hemorrhage according to the Heidelberg bleeding classification (9.6% vs 5.7%) and came with 11 procedure-related complications (6.9%)—one embolization in a previously uninvolved territory, two arterial dissections, two arterial perforations, and six “other” events. That last group included complications at the vascular access site in three patients and one case each of cerebral vasoconstriction, allergic reaction to contrast medium, and contrast medium-induced encephalopathy.
The benefits of thrombectomy clearly outweigh the potential risks in this “very severely affected” population, Thomalla said. The clinical message, he said, is that “we don’t have to care so much about the lesion volume itself, but about the overall situation of the patient where lesion volume is just one small part of it.”
Still, thrombectomy is just one aspect of care in this very sick group of patients, Thomalla indicated. “I think thrombectomy is one key feature that still shows that there is benefit to be gained by acute treatment, and everything else is then trying to avoid complications, the stroke unit treatment, and later on, of course, rehabilitation.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Costalat V, Jovin TG, Albucher JF, et al. Trial of thrombectomy for stroke with a large infarct of unrestricted size. N Engl J Med. 2024;390:1677-1689.
Disclosures
- The trial was supported by Montpellier University Hospital through an unrestricted grant from an industry consortium of medical device companies, including Medtronic, Stryker, Balt Extrusion, MicroVention, and Cerenovus.
- Costalat reports consulting for Balt USA, Johnson & Johnson Health Care Systems, Medtronic USA, MicroVention, Penumbra, and Stryker.
- Jovin reports having stock options from Anaconda, Basking Biosciences, FreeOxbiotech, Galaxy Therapeutics, Kandu, Methinks, Route92, and Viz.ai; holding stock in Gravity and StataDx; consulting for Cerenovus; and receiving grants/contracts from Medtronic and Stryker.




Comments