Low High-Sensitivity Troponin I Cutoff May Allow Discharge From ED for Many
Nearly half of patients had levels below 5 ng/L at presentation, and the rate of MI or cardiac death at 30 days was very low in this group.
ANAHEIM, CA—Patients with chest pain who present with a high-sensitivity cardiac troponin I level below 5 ng/L are good candidates for discharge from the emergency department, forgoing the need for resource-intensive admission and serial testing, a new systematic review suggests.
In pooled data from 19 cohort studies, that threshold had a negative predictive value of 99.5% for the primary composite outcome of MI or cardiac death at 30 days, Andrew Chapman, MD (University of Edinburgh, Scotland), reported at the American Heart Association 2017 Scientific Sessions. The findings were published simultaneously online in the Journal of the American Medical Association.
“The ability to use all of the data from all of the previous studies of high-sensitivity cardiac troponin I allowed us to really answer the question of what is the optimal threshold,” Chapman told TCTMD. “This analysis using studies with different prevalence of MI across different healthcare settings where there are quite significant differences in patient risk really gives us a considerable amount of confidence that this approach is safe, and it’s likely to give the guideline committees the evidence they require to consider recommending these strategies for clinical practice.”
He noted that there is now more evidence supporting risk stratification using a high-sensitivity troponin I cutoff of 5 ng/L—with discharge of patients with levels below that if no alternative causes of chest pain are found—than there was for using the 99th percentile as a threshold to diagnose MI when that concept was first introduced into guidelines.
Still, he added, there is a need for randomized data to confirm that implementation of such an approach is safe in everyday practice, because data have thus far come only from observational studies. To that end, Chapman’s research group is conducting the HiSTORIC trial in roughly 30,000 patients across Scotland, which should yield results next year. The trial will also allow for a formal cost-effectiveness analysis.
“We are as confident as we can be that based on the data available these strategies are safe, certainly a magnitude safer than using the 99th percentile to rule out patients at presentation to hospital, and we feel that there is a real potential to improve the efficiency and the cost-effectiveness of our practice without compromising patient safety,” Chapman said.
Homing In On the Right Threshold
Although prior studies have shown that patients with suspected ACS have a very low risk of adverse outcomes if they have a high-sensitivity troponin I level below 5 ng/L, the optimal threshold has remained uncertain.
In an attempt to bring the field to a consensus, Chapman and colleagues identified 19 relevant cohort studies involving risk stratification by high-sensitivity troponin I levels; they obtained patient-level data from 17 of them and aggregate data from the other two. The analysis included 22,457 patients in total, after exclusion of patients who presented with STEMI or cardiac arrest.
Nearly half of the patients (49%) had a troponin level below 5 ng/L at presentation, and in this group, there were very few primary outcome events: 59 index MIs, one MI at 30 days, and no cardiac deaths at 30 days.
The negative predictive value of using troponin I levels of less than 5 ng/L was high overall (99.5%), but lower values were seen in patients with myocardial ischemia on ECG (98.2%), those who presented within 2 hours of symptom onset (99.0%), those older than 65 (99.1%), and those with a history of ischemic heart disease (98.8%).
The researchers then compared cutoffs at 5 ng/L or 2 ng/L using patient-level data. The threshold of less than 5 ng/L—which encompassed 49.1% of patients—yielded a negative predictive value of 99.5%, missing 5.4 primary outcome events per 1,000 patients. The lower threshold had higher negative predictive value (99.8%), but it identified only 13.7% of patients as low risk and had a miss rate similar to that seen with the higher threshold (4.1 per 1,000 patients).
Thus, Chapman said, it makes more sense to use the cutoff of 5 ng/L because there is no disadvantage in terms of missed events and it allows for the identification of a much larger proportion of patients as candidates for early discharge from the emergency department.
“And when you apply it with the ECG, which is how we would advocate this is used in practice, you still identify 46% of all patients, which has the potential to significantly reduce healthcare expenditure and improve efficiency because we know that the admission or observation of patients with chest pain costs about $11 billion dollars in the United States every year,” Chapman told TCTMD. For patients presenting within 2 hours of symptom onset, he added, serial troponin testing is still recommended.
A Revolution, With Caveats
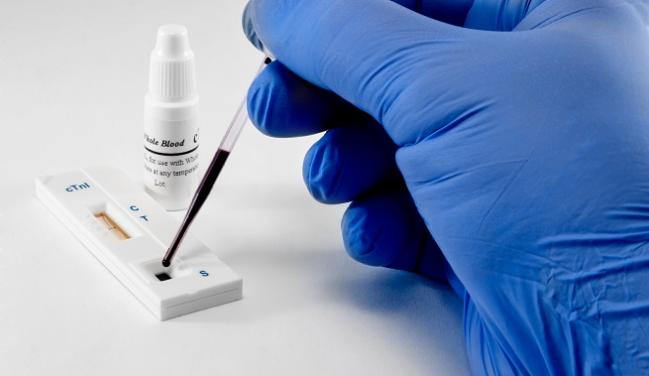
With US Food and Drug Administration approval of the Elecsys Troponin T STAT assay (Roche) in January, US physicians finally have access to the high-sensitivity troponin testing that has been available in other parts of the world for several years, and Umesh Khot, MD (Cleveland Clinic, OH), said that is changing how clinicians detect MI.
Commenting for TCTMD, Khot said his center has started developing algorithms to identify patients who are at very low risk using the high-sensitivity assay and who are candidates for discharge directly from the emergency department. “The patients are happier, and it also helps us in the sense of resource utilization because many hospitals are very tight for beds and capacity," he reported. "So if patients who don’t need to come into the hospital can be sent out, then this really helps as far as that.”
Asked whether there is enough evidence to support implementing the risk stratification approach advocated by Chapman’s group, Khot said there are some concerns when rolling this out in real-world populations.
First, he said, patients in everyday practice could have troponin distributions that differ from those seen in study populations.
Second, most studies have excluded early presenters (those with symptom onset within about 2 hours before presentation), and there is a concern about missing patients in this group who are at risk for future events using an approach like that studied by Chapman, he said.
And finally, there is a fear that because high-sensitivity assays are so valuable, a negative result could discourage further evaluation for conditions aside from MI, like pulmonary embolism, dissection, or other serious lung diseases, Khot said. “Sometimes this negative value can be too reassuring and people aren’t then worked up appropriately for other diseases.”
Although use of high-sensitivity troponin assays “is going to really revolutionize the treatment of these chest pain patients in the emergency department," he predicted, "I think that we do need to learn more, as we extend these data into real-life populations: what are some of the pitfalls and what are some of the issues.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Chapman AR, Lee KK, McAllister DA, et al. Association of high-sensitivity cardiac troponin I concentration with cardiac outcomes in patients with suspected acute coronary syndrome. JAMA. 2017;Epub ahead of print.
Disclosures
- The study was funded by the British Heart Foundation.
- Chapman reports being supported by a Clinical Research Training Fellowship from the British Heart Foundation and having received honoraria from Abbott Diagnostics and AstraZeneca.
- Khot reports no relevant conflicts of interest.


Comments