Lower Mortality With Complete Revascularization in Acute MI Patients With MVD
The patient-level meta-analysis takes the existing evidence to the next level, says Shamir Mehta.

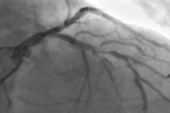
NEW ORLEANS, LA—Complete revascularization in patients presenting with ACS and multivessel coronary artery disease significantly cuts the risk of cardiovascular mortality and new MI when compared with a culprit lesion-only strategy, according to results from a large, patient-level meta-analysis.
Presented this week at the American Heart Association 2025 Scientific Sessions, the analysis also shows that a complete revascularization strategy cuts the risks of both cardiovascular and all-cause mortality.
“This takes the level of evidence to the next level,” lead investigator Shamir Mehta, MD (McMaster University/Hamilton General Hospital, Canada), told TCTMD. “This is one of the few instances where a PCI-based strategy has actually been shown to robustly reduce cardiovascular mortality. There are very few other indications for PCI in terms of reducing mortality.”
Even the COMPLETE trial, which randomized more than 4,000 patients in the largest randomized trial investigating complete revascularization to date, was underpowered to detect differences in mortality.
“Practice [has] largely shifted to performing complete revascularization, but there is still some skepticism about the robustness of the results,” said Mehta. “One thing that has not really been captured previously is whether it reduces mortality—cardiovascular mortality specifically.”
US guidelines contain a class 1 (level of evidence A) recommendation to perform complete revascularization for most patients with STEMI and multivessel disease to reduce the risk of death or MI and to improve angina-related quality of life. The European guidelines for ACS also recommend complete revascularization for hemodynamically stable STEMI patients with multivessel disease.
The new analysis, which was published simultaneously in the Lancet, included data from COMPLETE, FIRE, CvLPRIT, DANAMI-3-PRIMULTI, FULL REVASC, and Compare-Acute. In total, 8,836 patients (median age 65.8 years; 23.6% female) were randomly assigned to complete revascularization or culprit lesion-only PCI. In four of the studies, complete revascularization was performed using a physiology-guided approach. For timing, one study recommended nonculprit-lesion PCI during the index procedure, three trials recommended a staged approach, and two studies left the decision to operator discretion.
After a median follow-up of 360 months, the primary outcome of cardiovascular mortality or new MI occurred in 9% of patients treated with complete revascularization and 11.5% of those treated with culprit lesion-only PCI (HR 0.76; 95% CI 0.67-0.87). In terms of cardiovascular mortality, the rates were 3.6% and 4.6%, respectively (HR 0.76; 95% CI 0.62-0.93). The risk of new MI was cut by a relative 24% (HR 0.76; 95% CI; 0.65-0.90).
The risk of all-cause mortality dropped by a relative 15% with complete revascularization versus culprit lesion-only PCI (HR 0.85; 95% 0.73-0.99) and that benefit was driven by the reduction in cardiovascular mortality. Deaths from noncardiovascular causes were nearly identical, with Kaplan-Meier event curves that were “virtually superimposable,” said Mehta.
The reductions in cardiovascular mortality or new MI and cardiovascular mortality alone were consistent across a range of subgroups stratified by age, sex, STEMI vs NSTEMI, and angiography vs physiology guidance, among other categories.
The subgroup analyses are important, said Mehta, noting that the meta-analysis included more than 2,000 women. “Even in the really young patients with STEMI and multivessel disease, we saw a consistent reduction,” he said. “When you have diseases affecting younger patients, cardiovascular mortality becomes more and more important, so that’s a particularly important finding in this population.”
The ongoing prospective, multicenter COMPLETE-2 randomized trial will add to this space. Comparing a physiology-guided complete revascularization strategy to an angiography-based approach in 5,100 patients with acute MI and multivessel disease, the trial will use time to first occurrence of cardiovascular death or new MI as its primary endpoint. Mehta, who is the lead investigator, said recruitment should be completed by April 2026.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Mehta SR, Tiong DTW, Böhm F, et al. Complete versus culprit lesion-only revascularisation for acute myocardial infarction (Complete Revascularisation Trialists’ Collaboration): an individual patient-data meta-analysis of randomised trials. Lancet. 2025;Epub ahead of print.
Disclosures
- Mehta reports receiving an institutional grant from Abbott and consulting fees from Amgen, Janssen, Merck, Novartis, and Novo Nordisk.




Comments