More Data Hint at the Superiority of 3D Imaging for LAA Occlusion
Cases randomized to 3D CT used fewer devices and guides, took less time, and had more accurate device sizing compared with those guided by TEE.
Another study suggests that 3D imaging may lead to greater procedural efficiency and improved device selection accuracy for left atrial appendage (LAA) occlusions compared with the current recommendation of transesophageal echocardiography (TEE).
Last month, European data showed that operators performing the procedure blinded to TEE but using a system of 3D rotational angiography and fluoroscopy were able to effectively complete the occlusion in all but one of 20 patients.
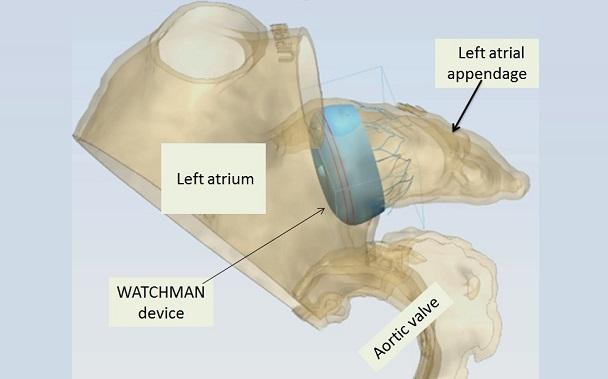
For the current study, published online last week ahead of print in Catheterization and Cardiovascular Interventions, Marvin Eng, MD (Henry Ford Health System, Detroit, MI), and colleagues randomized 24 patients who were undergoing LAA occlusion with the Watchman device (Boston Scientific) to a procedure guided by either 2D TEE or 3D CT. Both imaging modalities were used in all patients, but operators were blinded to the CT results in patients randomized to TEE.
All of the CT-guided procedures and 92% of the TEE-guided occlusions were deemed successful, but device selection on the first attempt was substantially better for the former cohort (92% vs 27%; P = 0.01). When intraprocedural upsizing was used in the TEE cohort, accuracy increased to 64% and there was no longer a significant difference (P = 0.33). Cases in which 3D CT was used required fewer devices (1.3 vs 2.5; P = 0.01) and guide catheters (1.0 vs 1.7; P = 0.01) and a shorter procedure time (55 vs 73 minutes; P < 0.05).
One stroke occurred over the course of the study in a patient randomized to the TEE arm.
“This study data supports the notion that comprehensive 3D assessment significantly simplifies [LAA occlusion], minimizing the time and number of steps needed,” Eng and colleagues write.
Maybe TEE Not The Best Way to Go?
Senior author of the aforementioned European study, Tom De Potter, MD (OLV Hospital, Aalst, Belgium), told TCTMD that these data combined with his team’s published findings “strongly suggest” the need for a larger study.
“What we haven’t had until now is strong evidence that there is a net clinical benefit for the patients,” he said. “Keep in mind the workflow we use for LAA closure has been studied and validated in thousands of patients. We studied 20 and these people studied 24, so it's proof of concept, but the proof of concept is solid across multiple studies [and] across multiple data sets, and it means that we need to go out and say that maybe TEE is not the best way to size the appendage to begin with.”
Maybe TEE is not the best way to size the appendage to begin with. Tom De Potter
Notably, the operators in the study “did not adhere tightly” to the manufacturer’s instructions for use sizing guidelines in the TEE cohort, the authors say. Despite this, 3D CT “demonstrated superior performance with respect to occluder accuracy and procedural efficiency.”
The decision-making, they add, “closely reflects clinical practice where device oversizing is common; thus, the maintained advantage of 3D CT remains broadly applicable.”
De Potter observed that “you obviously cannot blind the operator to the fact that there is no CT available to use, which means that the operators may tend to say they have only TEE imaging available and [since] they are susceptible to the idea that CT is better, they may say, ‘Okay, let's choose this device first.’ And if it turns out to be wrong they'll exchange it because we expect TEE to fail.”
Given that, he thought the number of devices used in the TEE arm was “unexpectedly high” compared with historical data suggesting this figure to be “closer to 1.2 or 1.3.” This is “a bit of a question mark for their data,” De Potter continued, “but I also don't think they aimed to prove anything conclusively in their data set.”
The “much more important message” for him is that this study confirms “what other authors have also observed and what we have seen: that a 3D imaging modality systematically sizes the appendage differently and gives you a larger value.” This is because “the way we size with 2D TEE is limited by the fact that you're taking some samples of a structure that is by nature very often not symmetrical. If your samples are not in the appropriate dimensions, you're going to miss part of the information,” De Potter explained.
Future studies should combine the methodology of this and his study by using randomization and having a study arm with no TEE, he concluded. “I do believe we'll be able to show a net clinical benefit for patients in terms of device exchanges and . . . procedural efficacy,” De Potter said.
Photo Credit: Dee Dee Wang, MD.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Eng MH, Wang DD, Greenbaum AB, et al. Prospective, randomized comparison of 3-dimensional computed tomography guidance versus TEE data for left atrial appendage occlusion (PRO3DLAAO). Catheter Cardiovasc Interv. 2018;Epub ahead of print.
Disclosures
- Eng reports serving as a proctor for Edwards Lifesciences.
- De Potter reports no relevant conflicts of interest.


joao tress