More Evidence Links Breast Arterial Calcification and CVD Risk
One author says the study, which ties BAC to subsequent ASCVD risk, should “move the needle” in terms of universal reporting.
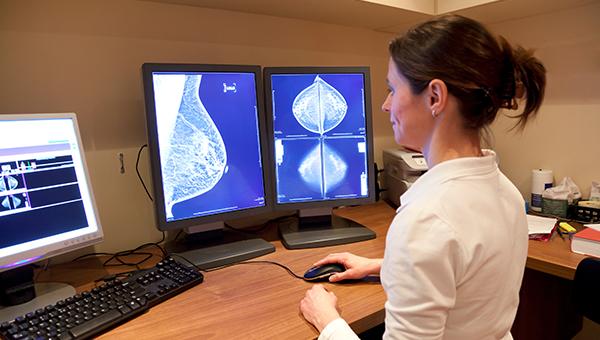
Calcification within the middle layer of the breast’s arterial wall found on digital mammography is associated with increased risk of atherosclerotic cardiovascular disease (ASCVD) and global CVD, according to a study of women in their 60s and 70s.
Investigators followed over 5,000 postmenopausal women for 6.5 years to see how the presence of breast arterial calcification (BAC), largely considered an incidental finding, correlated with CV outcomes.
“We found that women who had calcifications on a mammogram were at 51% increased risk of heart disease and stroke, and had a 23% increased risk of any form of cardiovascular disease,” senior study author Carlos Iribarren, MD, MPH, PhD (Kaiser Permanente Division of Research, Oakland, CA), told TCTMD. “This study, I think, moves the needle. Radiology should be reporting the presence and extent of breast arterial calcification on mammograms to women and to their primary care doctors.”
The study was published today in Circulation: Cardiovascular Imaging.
BAC is increasingly believed to be a marker of vascular aging and arterial stiffness. While prior studies have retrospectively examined the prevalence of BAC on mammograms and similarly proposed that radiologists should be universally reporting the presence of BAC on all mammograms, there remains no establishing role of BAC in CVD risk stratification, Iribarren said.
Some radiologists are already reporting BAC, but there is no guideline support or health insurance mandates requiring that it be reported or conveyed to patients, he added.
In an accompanying editorial, Natalie A. Cameron, MD, and Sadiya S. Khan, MD, MSc (both Northwestern University Feinberg School of Medicine, Chicago, IL), point to a recent survey of American College of Radiology members that found that up to 87% include BAC on mammography results, but only 41% said they do so “always” or “most of the time.” This contrasts with a survey of women, which found that 95% want to know their BAC status.
“While we still lack data that presence of BAC is ready for prime time to inform prevention decisions in women, BAC, as well as other areas of extracoronary calcification (ie, aortic and valvular), may serve as markers for underlying poor cardiovascular health,” Cameron and Khan write. Identification of BAC on a mammogram, they add, can serve as an opportunity to discuss shared upstream risk factors for both CVD and breast cancer.
Improved Risk Stratification
For the study, Iribarren and colleagues included women between the ages of 60 and 79 years who received at least one digital mammography screening between 2012 and 2015 and who had no prior CVD history or breast cancer.
BAC was present on 26% of mammogram reports. Compared with women lacking the calcification, those with BAC were older, more likely to be white or Hispanic, diabetic or prediabetic, and had higher systolic blood pressure, hypertension, and parity level.
This study . . . moves the needle. Radiology should be reporting the presence and extent of breast arterial calcification on mammograms to women and to their primary care doctors. Carlos Iribarren
Having BAC was associated with an increased risk of ASCVD (HR 1.51; 95% CI 1.08-2.11), the composite of acute MI, ischemic stroke, CVD death, as well as global CVD (HR 1.23; 95% CI 1.002-1.52), an endpoint that included ischemic heart disease, cerebrovascular disease, heart failure, cardiomyopathy, deep vein thrombosis\pulmonary embolism, cardiac arrest, peripheral arterial disease, retinal vascular occlusion, and CVD death. When BAC status was added to pooled cohorts equations risk, it improved model calibration and reclassification of ASCVD, with an overall net reclassification improvement (P = 0.01) as well as a bias-corrected clinical-net reclassification improvement (P = 0.04).
Iribarren and colleagues suggest that women with presence of BAC who have borderline or intermediate ASCVD risk may be candidates for more discussions and adjustments of preventive therapies, while those with BAC who are at high ASCVD risk may be candidates for more-aggressive therapy.
Another Piece of the Preventive Puzzle
Several findings from the study, say Cameron and Khan, suggest that BAC pathobiology is distinct from coronary artery calcification (CAC), a proven marker for CVD event prediction. One distinction is that women with BAC were not more likely to have higher rates of conventional ASCVD risk factors like smoking and high cholesterol.
“In addition, the authors did not find a dose-response relationship between BAC and CVD, as there is for CAC,” Cameron and Khan write. “ Although they noted a threshold effect for the 95th percentile of BAC on global CVD, similar results were not found for hard ASCVD, so the meaning of this threshold for ASCVD risk prediction remains unclear.
The editorialists point out, however, that with more than 70% of the older women in the study already on statins, and given known effects of statins on CAC growth and plaque repair, a dose-response for BAC may have been muted.
To TCTMD, Iribarren noted that BAC helped stratify 10-year ASCVD risk at every level, adding support for the importance of knowing BAC status. “This is bringing in another piece of the puzzle and we think [BAC] should be considered as a risk-enhancing factor,” Iribarren said. “Risk calculators are outdated, and they don't perform as well in women as they do in men. We need to recalibrate the models in contemporary populations.”
Iribarren added that his group next plans to assess BAC status in women in the 40- to 59-year age group to shed more light on its generalizability as a risk-enhancing factor.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Iribarren C, Chandra M, Lee C, et al. Breast arterial calcification: a novel cardiovascular risk enhancer among postmenopausal women. Circ Cardiovasc Imaging. 2022;15:e013526.
Cameron NA, Khan SS. Leveraging mammography as a unique opportunity for cardiovascular health promotion. Circ Cardiovasc Imaging. 2022;15:e013977.
Disclosures
- Iribarren, Cameron, and Khan report no relevant conflicts of interest.




Comments