Mystery MINOCA? Many COVID STEMIs Have No Culprit Lesion
Atypical rates of nonculprit STEMI have been seen in the NACMI registry, and the events are more common in women than men.

ATLANTA, GA—Patients who present with STEMI and a current or recent COVID-19 infection often have no culprit lesion, with a greater likelihood of this being the case in women than men, a prespecified analysis of the North American COVID-19 Myocardial Infarction (NACMI) registry shows.
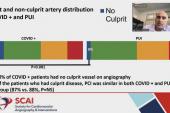
One-third of women and 18% of men had no culprit lesion detectable on angiography, a finding that the researchers say is “startling” considering that MI with nonobstructive coronary arteries (MINOCA) typically accounts for only 3.5% to 6.5% of all real-world STEMIs.
“MINOCA is always higher in women compared to men. We've known that from pre-COVID times,” lead study author Odayme Quesada, MD (The Christ Hospital Women’s Heart Center, Cincinnati, OH), told TCTMD. “But clearly COVID-19 is playing a role to dramatically increase the rates of these nonculprit STEMIs in women and men, and the question is why.” Quesada presented the findings today at the Society for Cardiovascular Angiography and Interventions (SCAI) 2022 Scientific Sessions.
Clearly COVID-19 is playing a role to dramatically increase the rates of these nonculprit STEMIs and the question is why. Odayme Quesada
Since the early days of the pandemic there have been uncertainties about how the virus contributes to systemic inflammation, with many patients found to have heightened risk for arterial or venous thrombotic complications. Quesada and colleagues say microvascular thrombosis and/or embolization is one potential mechanism for STEMI in patients with COVID-19 infection and no culprit lesion. Other possible causes range from stress cardiomyopathy in the setting of severe illness to disruption of coronary artery plaques, epicardial coronary spasm, spontaneous coronary artery dissection, and nonischemic cardiomyopathy.
Quesada and her group are stopping short of calling these findings MINOCA—because they are not sure that they are true MINOCA patients—preferring to refer to them as “nonculprit” STEMIs until they can get a better understanding of what is going on.
Commenting for TCTMD, Herb D. Aronow, MD, MPH (Henry Ford Health, Detroit, MI), called the mysterious findings “thought provoking,” adding that time will tell if microvascular thrombosis and other adverse pathology are at work that may contribute to a MINOCA-like STEMI. Both Quesada and Aronow said until more data are available, the possibility of a “COVID MINOCA” cannot be entirely ruled out.
“We have so few angiographic data on men and women with COVID and myocardial infarction,” Aronow said. “The NACMI registry has taught us a lot about the epidemiology, . . . but there is definitely more to learn.”
Parsing Sex Differences
The NACMI registry is a collaboration between SCAI, the American College of Cardiology, and the Canadian Association of Interventional Cardiology that includes hospitalized STEMI patients with COVID-19 from 64 medical centers in North America.
For the latest analysis, which focused on sex differences, Quesada and colleagues looked at in-hospital mortality in 585 patients (26.3% female) who were enrolled between March 2020 and late December 2021. All had tested positive for COVID-19 during or within 4 weeks before their index STEMI hospitalization. Compared with men, women were older and more likely to have preexisting diabetes and a history of stroke or TIA. All other risk factors were similar between men and women, and no significant sex-based differences were seen in pre-PCI cardiac arrest, cardiogenic shock, or left ventricular ejection fraction.
Primary or rescue PCI was performed more in men than women (76% vs 61%; P = 0.002), with women more likely to receive medical therapy (33% vs 20%; P = 0.003). There were no sex differences in average length of stay, proportion of CABG, use of thrombolytics, or door-to-balloon time.
The NACMI registry has taught us a lot about the epidemiology, . . . but there is definitely more to learn. Herb Aronow
In all, 33% of women and 27% of men died while hospitalized (P = 0.22), with no significant sex differences in rates of stroke, reinfarction, or the composite endpoint of in-hospital death, stroke, or reinfarction. Adjustment for angiographic and clinical factors did not change the results.
The high rates of death are in line with prior reports from a larger NACMI cohort showing a 33% mortality rate in men and women with STEMI and COVID.
Aronow added that while the NACMI data are “fairly representative” of the clinical experience of STEMI in the setting of COVID, the numbers of patients are too small to draw firm conclusions. However, he noted that the registry does seem to be showing an interesting shift away from chest pain and toward dyspnea as the dominant presenting symptom for women, rather than chest pain, which was the predominant presenting symptom for both sexes pre-COVID. Women in NACMI presented with dyspnea at a rate of 56%, compared with 45% for men (P = 0.02).
However, Aronow cautioned that “the jury is still out on whether or not there really are differences in outcomes between men and women with COVID who suffer myocardial infarction.”
Looking Toward Additional Insight
In an editorial accompanying the study, Mirvat Alasnag, MD (King Fahd Armed Forces Center, Jeddah, Saudi Arabia), and colleagues say understanding key causes of MINOCA in COVID will require ongoing work and may benefit from the use intracoronary imaging, provocative testing, cardiac MRI, and thrombophilia assays.
“Although NACMI lacks adjudication of outcomes, it is a representation of disease patterns and practice trends,” they write. “The NACMI sex substudy provides an incentive to understand MINOCA further and press clinicians to investigate these cases more accurately.” Importantly, Alasnag and colleagues say as the registry grows, “analyzing outcomes by race/ethnicity and sex may provide additional insight into any potential disparities of care.”
Quesada said the next step is core-lab analysis to try to get to the bottom of whether these are true MINOCAs or MINOCA mimickers. “We just don’t know enough at this point to say for sure,” she added. Also important will be to get enough vaccinated patients into the registry to compare their outcomes with the early-pandemic patients. Only 22 patients in the current analysis were vaccinated and none of them died, which was reported previously in another NACMI analysis that showed in-hospital mortality dropping by about 25% between 2020 and 2021.
Given observations of STEMI mimics in COVID patients, panelist Jacqueline Tamis-Holland, MD (Icahn School of Medicine at Mount Sinai, New York, NY), asked if any of the patients with the MINOCA-like STEMIs had cardiac MRI to differentiate whether there might be nonischemic mechanisms at play.
Quesada said given the COVID-positive status of these patients, chances are slim that many cardiac MRIs were done, but the echocardiographic data will help determine how many might be Takotsubo.
Panelist Gregg Stone, MD (Icahn School of Medicine at Mount Sinai), added that while the study raises a host of questions, he thinks there is a good possibility that some of the cases are type 2 MIs, or demand-ischemia MIs. Quesada said that issue will be addressed by evaluation of the ECGs to confirm that true ST elevations occurred.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Quesada O, Van Hon L, Yildiz M, et al. Sex differences in clinical characteristics, management strategies, and outcomes of STEMI with COVID-19: NACMI registry. JSCAI. 2022;Epub ahead of print.
Alasnag M, Shah B, Botti G, et al. STEMIs and a closer look at MINOCA during the COVID-19 pandemic. JSCAI. 2022;Epub ahead of print.
Disclosures
- Quesada reports research grants from Edwards Lifesciences, Boston Scientific, Medtronic, and Abbott Vascular; and consulting for Medtronic and Boston Scientific.
- Alasnag and Aronow report no relevant conflicts of interest.




Comments