NeuroARC Proposes New Standards for Assessing Neurologic Damage in CV Clinical Trials
Beyond stroke, the endpoints capture damage that is less obvious but can have a lasting impact on patients’ day-to-day function, researchers say.
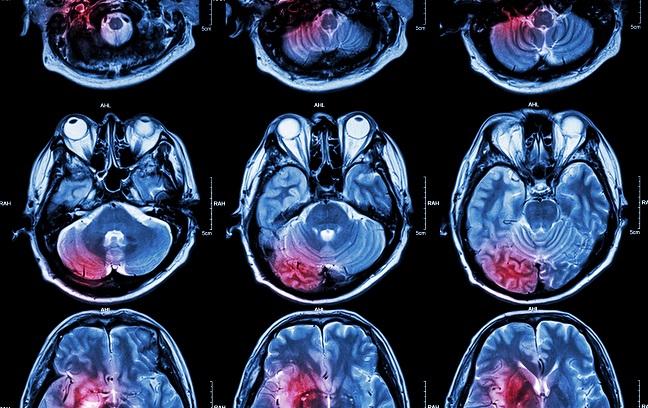
The Neurologic Academic Research Consortium (NeuroARC) has released standardized endpoints for assessing how the brain functions after surgical or catheter-based cardiovascular interventions. Meant for use in clinical trials, the endpoints cover not only more obvious harm to neurologic function but also “covert” damage.
Details on the NeuroARC initiative, which involved collaboration among US and European physicians, researchers, regulatory experts, and industry representatives, were published online February 6, 2017 in the Journal of the American College of Cardiology.
“The neuroprotective goal of some cardiovascular procedures, as well as the broader iatrogenic risks, mean that neurologic and cognitive outcomes should be a fundamental part of the dialogue between physicians and patients when choosing a management strategy that is aligned with that individual’s preferences,” lead author and NeuroARC co-chair Alexandra Lansky, MD (Yale University, New Haven, CT), told TCTMD in an email.
“We hope that standard definitions and assessments will help clarify the true benefit-risk ratio of various therapies and ultimately lead to better-informed decisions and better outcomes for patients,” she said.
In a press release, Michael Mack, MD (Baylor Scott & White Health, Dallas, TX), also a NeuroARC co-chair, described the value of capturing more subtle events.
“Until now, many studies evaluating the safety of TAVR and other cardiovascular procedures only recorded the most devastating strokes, which meant that doctors—and their patients—were unaware of the full risk potential,” he said. “We hope this paper will cause researchers to report their findings in a more comprehensive and consistent way so that clinicians can properly interpret the results to provide the best care to patients.”
Damage Across a Spectrum
Procedure-related stroke manifests in various ways and is “substantially underreported,” the paper notes, “and systemic evaluations by neurologists commonly uncover more subtle, but nonetheless clinically significant, neurologic deficits.”
Silent ischemic infarcts affect an estimated 600,000 patients each year in the United States, Lansky and colleagues report. Thus, they say, “a better understanding of their clinical implications, and the role of imaging and cognitive measures in device and procedural evaluations, is necessary.”
The NeuroARC document breaks neurological endpoints into three categories:
- Type 1: Overt damage to the central nervous system (CNS) with acutely symptomatic brain or spinal cord injury
- Type 2: Covert CNS injury involving acutely asymptomatic brain or spinal cord injury detected by neuroimaging
- Type 3: Neurologic dysfunction (acutely symptomatic) without detectable CNS injury
In addition, it specifies two composite endpoints: CNS infarction and CNS hemorrhage. Another element is an overview of how and when such injuries and cognitive outcomes are assessed in clinical trials based on the device or procedure being studied.
“This document represents a multispecialty consensus that harmonizes several sets of definitions that were designed for different purposes, and we think they are a very solid foundation as this field matures,” Lansky noted to TCTMD, predicting that some aspects will be refined as data and insight are generated.
“We anticipate early adoption of these new standards, as in most instances they will increase the power of trials evaluating neurological events as primary safety or efficacy endpoints, and in general I think the utility of more sensitive measures of these important outcomes will be readily apparent,” she said.
There is built-in flexibility when it comes to ascertainment so that use of the endpoints “is not overly burdensome and is tailored to each study,” Lansky added. “These definitions have already been incorporated into ongoing trials of cerebral protection, as well as planned trials evaluating left atrial appendage closure devices, and I expect we’ll begin to see at least short-term outcomes according to these definitions early next year.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Lansky AJ, Messé SR, Brickman AM, et al. Proposed standardized neurological endpoints for cardiovascular clinical trials: an Academic Research Consortium initiative. J Am Coll Cardiol. 2017;69:679-691.
Disclosures
- Lansky reports receiving research grant support from Keystone Heart, NeuroSave, and Boston Scientific, as well as speaker/consultant fees from Keystone Heart.


Comments