A New Biomarker to Diagnose Acute Myocarditis?
The microRNA’s specificity to myocarditis is unique, and “that would make it a very powerful tool,” a researcher says.

A novel microRNA measured in plasma, first discovered in mice and then isolated in humans for the first time, eventually might provide a simpler way to diagnose acute myocarditis, a preliminary study suggests.
Expressed by type 17 helper T (Th17) lymphocytes, levels of the microRNA accurately distinguished patients with acute myocarditis from those with acute MI, with an area under the receiver-operating-characteristic curve (AUC) of 0.927, according to researchers led by Rafael Blanco‑Domínguez, MSc, and Raquel Sánchez‑Díaz, PhD (both National Center for Cardiovascular Research, Madrid, Spain).
The biomarker’s ability to identify patients with acute myocarditis was confirmed through comparisons with other groups of patients, as well, including those with MI with nonobstructive coronary arteries (MINOCA) and a variety of autoimmune diseases, the investigators report in a study published in the May 27, 2021, issue of the New England Journal of Medicine.
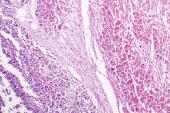
An easy-to-measure diagnostic biomarker would be welcome for acute myocarditis, which can mimic MI, making it challenging to come to a definitive diagnosis. The gold standard is endomyocardial biopsy, but its invasive nature is a drawback. Acute myocarditis can also be identified using cardiovascular magnetic resonance (CMR) imaging, but that isn’t available at all centers. “Therefore, reliable and accessible diagnostic tools for the early diagnosis of acute myocarditis are an unmet clinical need,” the authors say.
Study author DeLisa Fairweather, PhD (Mayo Clinic, Jacksonville, FL), told TCTMD that “by having a biomarker like this that could be rapidly examined, this would be a distinguishing way to understand that this is myocarditis versus a myocardial infarct versus potentially some other kind of heart disease.”
Fairweather said this microRNA—dubbed hsa-miR-Chr8:96—is unique in that it is specific to myocarditis, which contrasts with other CV biomarkers like troponin, which can reflect damage related to a variety of conditions. “That would make it a very powerful tool,” she said.
The Potential of MicroRNAs
MicroRNAs, the researchers note, “have emerged as innovative biomarkers for cardiovascular disease.” They initially identified the biomarker in this study by examining microRNAs expressed by circulating T cells in mouse models of autoimmune or viral myocarditis. Expression of this microRNA enhances the proautoimmune activity of T lymphocytes and contributes to the severity of inflammation in the myocardium, senior author Pilar Martín, PhD (National Center for Cardiovascular Research), explained to TCTMD.
The team “confirmed that Th17 cells, which are characterized by the production of interleukin-17, are a characteristic feature of myocardial injury in the acute phase of myocarditis,” they write in their paper. “The microRNA mmu-miR-721 was synthesized by Th17 cells and was present in the plasma of mice with acute autoimmune or viral myocarditis but not in those with acute myocardial infarction.”
Next, the investigators identified the human homologue for this microRNA, hsa-miR-Chr8:96, confirming that it was present in four independent cohorts of patients with myocarditis. They found that plasma levels among 42 patients with myocarditis were higher than those seen in 90 patients with MI and 80 healthy participants.
“We analyzed additional validation cohorts with different comparators, which confirmed that the novel miRNA was specifically expressed in plasma from patients with myocarditis, as compared with those with myocardial infarction or MINOCA,” the authors write. “These data were also validated in a cohort of patients with biopsy-proven myocarditis, along with patients who had other Th17-related diseases (rheumatoid arthritis, spondyloarthritis, psoriasis, and multiple sclerosis).”
It would be very nice to have diagnosis by a blood test instead of needing very expensive techniques like magnetic resonance or very aggressive tests like biopsy. I think it’s the future of diagnosis. Pilar Martín
The microRNA’s high diagnostic value for distinguishing acute myocarditis from acute MI remained in models adjusted for age, sex, ejection fraction, and serum troponin levels. That’s important because myocarditis is a male-dominant disease that tends to occur in younger individuals, Fairweather said. She added that the findings regarding the performance of the microRNA indicate that “there might be sex and age differences in it, but it still looks like it’s going to be useful in spite of those differences.”
Next Steps
Several issues remain to be investigated before this novel biomarker reaches clinical applicability. The researchers note in their paper that “great variability” in the expression of hsa-miR-Chr8:96 remains unexplained. “It is not clear whether this variation reflects the severity of the disease or is attributable to some other factor,” they say.
Martín said national-level registries have been launched to compare use of the biomarker with current diagnostic methods for myocarditis, and it is hoped that the microRNA can be validated for clinical use over the next 2 years.
Additional research is needed, too, to see whether this novel biomarker can discriminate between patients with myocarditis and those who have progressed to dilated cardiomyopathy, Fairweather said. She added that a clinically useable assay to measure the microRNA—with an established diagnostic cutoff—is needed.
If the microRNA is ultimately validated and brought to the clinic, it could represent a paradigm change in how cardiovascular diagnoses are made, Martín said. “I think that this is a new [opportunity] in the cardiovascular area that we need to push at,” she elaborated. “We have published now this microRNA for this disease, but we are investigating others that can help to distinguish between the different cardiomyopathies, and it would be very nice to have diagnosis by a blood test instead of needing very expensive techniques like magnetic resonance or very aggressive tests like biopsy. I think it’s the future of diagnosis.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Blanco‑Domínguez R, Sánchez‑Díaz R, de la Fuente H, et al. A novel circulating microRNA for the detection of acute myocarditis. N Engl J Med. 2021;384:2014-2027.
Disclosures
- The study was supported by grants from the Ministry of Science and Innovation through the Carlos III Institute of Health – Fondo de Investigación Sanitaria, the Biomedical Research Networking Center on Cardiovascular Diseases, Comunidad de Madrid, Fundació La Marató de TV3, the European Research Council, Fondo Europeo de Desarrollo Regional, and the BBVA Foundation. The National Center for Cardiovascular is supported by the Carlos III Institute of Health, the Ministry of Science and Innovation, and the Pro CNIC Foundation, as well as by a Severo Ochoa Center of Excellence grant.
- Martín and Sánchez‑Díaz report patents for methods for the diagnosis of cardiomyopathies.
- Fairweather reports grants from the US National Institutes of Health.
- Blanco‑Domínguez reports a grant from the Formación de Profesorado Universitario program of the Spanish Ministry of Education, Culture, and Sports.




Comments