Non-COAPT-Like Patients Fare Well With MitraClip, EXPAND Suggests
Registry results imply that HF patients who wouldn’t have been eligible for COAPT—even the very sick—did well with TEER.
Chicago, IL—Real-world patients with mitral regurgitation (MR) not meeting the COAPT eligibility criteria who ultimately underwent clip-based transcatheter mitral valve repair fared just as well as COAPT-like patients meeting the strict trial requirements who also received the device, according to data from a new registry.
Use of MitraClip (Abbott) in symptomatic patients with only moderate MR, as well as in those with advanced heart failure, led to sustained improvements in MR and functional class, report investigators. Both groups of patients would have been excluded from the COAPT randomized trial comparing MitraClip against medical therapy in secondary MR.
Additionally, clinical outcomes at 1 year were on par with COAPT-like patients who received the device.
The registry data, say investigators, shed light on use of MitraClip outside the clinical trial setting and the results operators are achieving in the real world.
“What I was most struck by was the reduction in MR at 1 year,” lead investigator Gilbert Tang, MD, MBA (Icahn School of Medicine at Mount Sinai, New York, NY), told TCTMD. “It was a sustained reduction in the COAPT-like patients, which is encouraging because these patients are supposed to be similar to the COAPT trial patients, as well as in the other [non-COAPT-like] patients.”
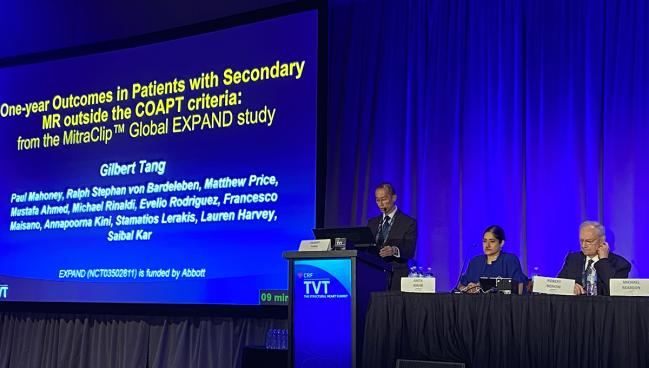
Tang presented the results from the global EXPAND registry study during a late-breaking clinical trial session at TVT 2022. The registry was designed to evaluate the prevalence and outcomes of secondary MR patients outside the COAPT eligibility criteria treated with MitraClip. He noted that the advanced heart failure (HF) patients included in EXPAND were extremely sick with limited treatment options.
“All of these patients are symptomatic—that’s why they’re being treated,” said Tang. “The question is whether they are too late to be treated.”
COAPT: Strict Inclusion Criteria
The COAPT trial, published in the New England Journal of Medicine in 2018, was the landmark study that led to an expanded indication for transcatheter edge-to-edge repair (TEER) in HF patients with moderate-to-severe functional MR (≥ 3+) despite treatment with optimal medical therapy.
Inclusion criteria for the trial were strict, as previously reported by TCTMD, and those tight criteria are typically cited as a key reason why COAPT results differed from those of the other randomized clinical trial in this space, MITRA-FR. COAPT included symptomatic patients with HF and moderate-to-severe MR despite being aggressively treated with guideline-directed medical therapy (GDMT), and patients were randomized to MitraClip plus GDMT or medical therapy alone. All patients were required to have an LVEF ranging from ≥ 20% to ≤ 50% and left ventricular end-systolic dimension (LVESD) ≤ 70 mm.
As part of the EXPAND registry, which is a prospective, observational, postmarketing study of patients treated at 57 sites in seven countries, 1,041 subjects with site-reported MR 3+/4+ were enrolled and received the MitraClip. Of these, researchers analyzed data on 413 subjects with echocardiographic core-lab assessed functional MR who received the device.
The cohort included 125 patients classified as COAPT-like, meaning they met the eligibility criteria from the randomized trial. Additionally, 128 subjects were classified as non-COAPT-like with moderate MR only (NCL-MMR). These patients had core-lab assessed MR 2+ at baseline and at least one of the following criteria: LVEF ≥ 20%, LVESD ≤ 70 mm, or systolic pulmonary artery pressure (PAP) ≤ 70 mm Hg. Finally, the cohort also included 32 non-COAPT-like patients with advanced heart failure and severe MR at baseline (NCL-AHF). In addition to MR 3+/4+, they had to have at least one of the following criteria: LVEF < 20%, LVESD > 70 mm, or systolic PAP > 70 mm Hg.
At baseline, there were no significant differences in the use of HF medications between the COAPT-like and non-COAPT-like patients. However, one of the limitations of the analysis, as Tang pointed out, is that drug dosages are not recorded in the EXPAND registry.
At 1 year, MR was reduced to mild or less (≤ 1+) in 86.5% of the COAPT-like patients treated with MitraClip. Comparatively, 97.2% of the NCL-MMR patients treated with MitraClip had their MR reduced to mild or less. Among the advanced HF patients, 81.3% had their MR reduced to mild or less at 1 year. In terms of NYHA functional class, 81% of the COAPT-like patients, 83% of the NCL-MMR patients, and 77% of the NCL-AHF patients were in class I/II at 1 year, and these changes were statistically significant compared with baseline. All three groups reported significant improvements in quality of life from baseline to 1 year.
“In the non-COAPT-like patient with moderate MR, they had healthier ventricles, smaller ventricles,” said Tang. “As a result, the MR reduction is better—97% at 1 year, which is important because it was reduced to 1+. We’re not talking about 2+ being a win anymore, we’re talking about 1+ being a win. We know from other studies that the less residual MR the patient has, the better the outcomes. Same thing with the advanced heart failure group, which was a very heterogenous population. Here, reducing MR did help them functionally and their NYHA class and [quality of life] improved. The MR wasn’t as good as the other group, but at 1 year, it was still 81%, which was still a win.”
Of the COAPT-like patients, 22.6% had died at 1 year and 32.6% had been hospitalized for HF. Among the NCL-MMR patients, rates of mortality and hospitalization for HF at 1 year were 19.6% and 25.0%, respectively (P = NS compared COAPT-like patients). Similarly, in the advanced HF patients, 22.8% had died at 1 year and 24.5% had been hospitalized for HF (P = NS compared with COAPT-like patients).
To TCTMD, Tang stressed the need for a deeper dive into the data to understand what factors are driving clinical outcomes, particularly given the heterogeneity of the advanced HF group. He also noted that despite being published not quite 4 years ago, COAPT is a “historical trial” given how fast the field of HF is evolving with new therapies, including the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors. The new therapies, said Tang, provide clinicians with greater options for managing the ventricular dysfunction of secondary MR while the addition of MitraClip appears to allow physicians to reduce MR to 1+ and keep it there.
Finally, Tang noted there is a need to study if the outcomes achieved in this analysis can be improved upon with the introduction of the MitraClip G4, the latest iteration of the device.
What Advanced HF Patients Would Benefit?
Anita Asgar, MD (Montreal Heart Institute, Canada), one of the panelists for the session, highlighted the lower rate of HF hospitalizations among the advanced HF patients compared with the COAPT-like patients, and wondered if there was any potential downside of treating such patients given the safety of MitraClip.
“In the advanced heart failure population, it’s quite a heterogenous group,” Asgar told TCTMD, “but there was clearly a benefit in heart failure hospitalizations. There is other data suggesting there is that benefit, but it’s still difficult to tease out which group of patients we should try [with MitraClip]. It’s a small number of patients [with advanced HF] and I think there is going to be a benefit in this group, but we need more data. And it all comes down to your outcome of interest. Is it mortality? You’re probably not going affect mortality because that train has left the station, but if you can improve heart failure hospitalization and quality of life, who is to say there’s not a benefit there?”
Ran Kornowski, MD (Rabin Medical Center/Beilinson Hospital, Petah Tikva, Israel), said the new analysis “raises a lot of questions” given that MitraClip is currently not recommended for patients who wouldn’t meet the COAPT eligibility criteria.
“But they were treated, which means there was something that made the operator or team to refer these patients for the clip,” he said. “So what is external validity of this group compared with a much larger group of patients with moderate MR or severe heart failure who have not been treated?”
Tang agreed that that remains to be seen, noting that the present analysis is hypothesis-generating and use of MitraClip in these non-COAPT-like patients should be studied more directly, particularly since those with severe MR and advanced HF represents a large patient population. He also pointed out that all patients were symptomatic with site-reported MR 3+/4+, meaning the clinicians on the heart team felt such patients closely matched with the COAPT criteria and could benefit from the device.
Asgar noted there is also a strong interest in the treatment of moderate secondary MR, noting they are currently conducting the EVOLVE-MR study, which is studying whether an earlier intervention can slow the progression of disease in patients.
“Can we prevent the further deterioration of LV function by doing a very safe procedure?” said Asgar. “You wouldn’t operate on these patients because of the morbidity but if you could do a transcatheter procedure, they go home in 24 hours, and you delay the progression of disease, why not? It’s something to study.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Tang G, Mahoney P, von Bardeleben RS, et al. One-year outcomes in patients with secondary MR outside the COAPT criteria: the MitraClip Global Expand study. Presented at: TVT 2022. June 8, 2022. Chicago, IL.
Disclosures
- Tang report consulting/honoraria/speaker’s bureau fees from Abbott Vascular, Medtronic, NeoChord and serving (unpaid) on an advisory board for JenaValve.
- Asgar report grant support/research contract with Abbott Vascular. She reports consulting/honoraria/speaker’s bureau fees from Medtronic, Edwards Lifesciences, and W.L. Gore.
- Kornowski reports no conflicts of interest.




Comments