OCT Guidance Cuts Stent Use in STEMI Without Plaque Rupture: EROSION III
In theory, plaque erosion, not a rupture, could be left unstented, but the need for dual antiplatelet therapy likely persists.
(UPDATED) Using optical coherence tomography (OCT) guidance to determine that a STEMI patient does not, in fact, have an occlusive lesion can significantly reduce the rate of stent implantation without increasing short-term MACE, results of the EROSION III study show.
“OCT can be considered for decision-making in customizing and optimizing the reperfusion strategy for STEMI patients,” said Haibo Jia, MD, PhD (Second Affiliated Hospital of Harbin Medical University, China), who presented full results from EROSION III during a late-breaking clinical science session later in the day.
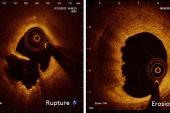
The idea for the trial stems from the observation that a small subset of patients, particularly younger ones, may present with classic STEMI symptoms but after aspiration thrombectomy are found to have plaque erosion, not a ruptured plaque, and at least theoretically, no need for a stent and its attendant dual antiplatelet therapy (DAPT).
The first, single-center, proof-of-concept EROSION study in 2016, reported by TCTMD, suggested ACS patients screened by OCT and found to have plaque erosion, not rupture, could safely be treated with antithrombotics instead of stenting without increasing short-term recurrent ischemic events. One-year results, subsequently published in Circulation: Cardiovascular Interventions, showed that most of the 53 patients who’d completed 12-month follow-up and were managed with aspirin and ticagrelor without stenting remained free of major adverse cardiovascular events.
But the notion that stents might not always be needed is one that many in the field have found hard to wrap their heads around: in 2019, a Times of India article suggesting that intravascular imaging could bid “goodbye to stents” produced an outcry on Twitter when the headline was widely retweeted.
EROSION III Results
For EROSION III, 246 STEMI patients were randomized and underwent initial angiography and thrombus aspiration (if needed). Those with TIMI 3 flow and a stenosis of 70% or less were randomized 1:1 to OCT guidance followed by “mechanism-based” management (n = 112), or to standard care based on angiographic guidance (n = 114). In the OCT group, a decision not to stent could be based on evidence of plaque erosion, spontaneous coronary artery dissection (SCAD), or plaque eruption without dissection.
The primary efficacy endpoint, reduction in stent implantation, was met: just 43.8% of patients in the OCT-guidance arm ultimately got a stent as compared with 58.8% in the angiography group, a significant 15% difference. For the cohort as a whole, plaque erosion was identified in 26% of patients, and the majority of these (86%) were treated conservatively in the OCT guidance group, as compared with 14% in the angiography-guided group.
For the primary safety endpoint, investigators saw no significant difference in MACE-free survival at 30 days, although the trial was not powered for this endpoint. Of note, by the 1-year mark, five patients (7.9%) in the OCT arm and four patients in the angio-only arm (8.5%) who were not stented at the outset ultimately required target lesion revascularization.
Some Context on Concept
Discussing the results with TCTMD, Ziad Ali, MD, DPhil (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), credited the EROSION investigators for chipping away at an “interesting concept” with this series of trials.
“We're moving more towards understanding the plaque biology instead of just going ahead and putting in stents without thinking about it,” he said. “What is reassuring is that their rate of finding mechanisms of myocardial infarction that are not plaque rupture is consistent with the literature, but it also serves as a refresher that not all heart attacks are because of a plaque rupture. About 35% are not.”
An erosion, Ali explained, is essentially a section of endothelium that gets denuded—something that’s especially common in younger smokers, in patients with diabetes, and in perimenopausal women as estrogen levels change. When these erosions occur, the vessel “becomes kind of like a gravel road and that gravel is really sticky for the platelets.”
That poses something of a catch-22, he continued, since a key rationale for using OCT is to avoid the need for a stent and its attendant dual antiplatelet therapy. But the presence of thrombus and the persistence of a section of vessel prone to attracting platelets remains, he explained.
“There clearly is a thrombus as a mechanism of either erosion or these calcified nodules, so they still need DAPT,” said Ali. “So what do you really save? You save the potential harm or impact of a stent, which is somewhere about 5% in contemporary trials.”
Moreover, skipping the stent by using OCT is unlikely to save money in most cath labs, Ali pointed out. “An OCT catheter in India is about $1,500, and the stent is like a hundred bucks.”
Overall, said Ali, “if you're looking for a reason to not stent and to reassure yourself that that’s okay, then this study achieved its aim.” Looking at the bigger picture, he added, EROSION is provocative in that it does run counter to the dominant primary PCI strategies of recent years, which are solidly stent-based.
“Balloons aren't what they were in 1995,” he said, “and we may not need to stent all vessels because biology is changing and our understanding of the biology of heart attacks is changing and the tools that we have to be able to investigate these are now available and we should use them. We're still in the learning process, but simply putting a stent into every vessel clearly isn't the way forward.”
Comfort Level
During a discussion following the press conference, moderator Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), addressed the issue of operator comfort in leaving the vessel alone, even after thrombus aspiration. “If you do not have imaging on board, I don’t think you can feel comfortable in leaving [it alone], even after thrombus aspiration, [but] if you actually have imaging, that's when you would feel more competent not placing stents.”
This is particularly important in younger women, Mehran added, who might be particularly at risk for SCAD.
Shmuel Banai, MD (Tel Aviv Medical Center, Israel), agreed. “Because of this uncomfortable feeling, we always bring patients back after a week or 10 days to look at the artery and make sure it’s completely patent.” The 40% rate of non-stenting in the angiography group was “very high,” he noted, to which Jia replied that in this arm, the majority of patients not treated with a stent had stenoses of less than 50%.
Banai, to TCTMD, said that in most cath labs, the rate of STEMI patients ultimately not stented would be vastly smaller—in his cath lab, it ranges from zero to 5%.
A separate issue, raised both in the press conference and in the study’s main presentation, was the high use of thrombus aspiration, prompting discussant Jennifer A. Rymer, MD, MBA (Duke University, Durham, NC), to point out that thrombectomy is considered a class III recommendation (of no benefit) in US STEMI guidelines.
Jia, who had reported that rates of thrombectomy were 92% and 95.6% in the OCT and angiographic groups, respectively, said that patients were specifically chosen because they had large thrombus burden, and that imaging indicated that high-quality thrombus aspiration clearly reduced stenosis in both groups. “Of course, we are concerned . . . that thrombectomy is not recommended as a routinely used technique in primary PCI, but at least for these selected patients it may of benefit for reduction of thrombus burden and restoring antegrade blood flow,” he reassured.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Jia H, Dai J, He L, et al. OCT-guided intervention in STEMI with early infarct artery patency (EROSION III): a multicenter randomized controlled trial. Presented at: TCT 2021. Orlando, FL. November 4, 2021.
Disclosures
- Yu and Jia report no relevant conflicts of interest.
- Ali reports serving as the principal investigator for the Abbott-sponsored ILUMIEN trial.
- Banai reports serving as a medical director for Neovasc.
- Mehran reports grant support/research contracts (institutional) from Abbott Vascular, AstraZeneca, Bayer AG, Bristol-Myers Squibb, CSL Behring, Daiichi-Sankyo/Eli Lilly and Company, Medtronic, Novartis Pharmaceuticals, OrbusNeich, CERC, Chiesi, Concept Medical, Applied Therapeutics, Beth Israel Deaconess, Zoll, Arena, Biosensors, Boston Scientific, CellAegis, Insel Gruppe AG, Philips, and Transverse Medical; consultant fees/honoraria/speakers bureau fees (personal) from Medscape/WebMD, Janssen Scientific Affairs, Cine Med Research, ACC, CIRM, SCAI, and WebMD; equity < 1% (personal) from Elixir Medical, Applied Therapeutics, and STEL; equity < 1% to her spouse (personal) from ControlRad; advisory board payments (institutional) from Idorsia Pharmaceuticals; scientific advisory board payments (personal) from the AMA; consultant fees/honoraria/speakers bureau fees (institutional) from Abbott Vascular, Abiomed, AM-Pharma, Alleviant, Bayer, Beth Israel Deaconess, CardiaWave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; divested equity < 1% (institutional) from Claret Medical (now Boston Scientific); and scientific advisory board payments to her spouse (personal) from Biosensors.


Comments