Twitter Takes on the Times of India, but the Question Persists: Is Foregoing a Stent an Option?
A news headline sparked a Twitter outcry, but some say the best tactic for plaque erosion seen on OCT needs sober consideration.
As tweets go, it was innocuous enough. “What gets published in the @TimesofIndia,” Purvi Parwani, MD (Loma Linda University Health, CA ), tweeted last month, along with a photo of a clipping from the March 24, 2019, Sunday edition of the Mumbai-based newspaper.
“Now Chembur Hospital Doc Says Goodbye to Stents, Blood Thinners,” the headline announced, followed by the slug: “Near Infrared Light Looks Inside Heart Arteries.”
The tweet sparked a blaze of opinions that, as she told TCTMD, caught even Parwani off guard. Many responses decried the inappropriateness of the headline and demanded that the Times of India retract the article. A few tweeters, however, waded cautiously into the fray to remind cardiologists of an uncomfortable truth: there are data—albeit limited—that certain MI patients, especially young ones, might be better off without stents. They said the concept at the heart of the newspaper story should not be dismissed out of hand.
The Times article describes the case of three acute MI patients, two in their 20s and one in her 30s, all admitted with acute MI to the Surana Hospital in Chembur, a suburb of Mumbai. In all three cases, optical coherence tomography (OCT) imaging was used to determine that the patients had thrombi, not plaque rupture, and all three were treated with thrombolysis instead of a stent.
“We are planning to conduct a research study looking at heart attacks among the young using OCT,” Surana Hospital cardiologist VT Shah, MD, is quoted in the article as saying. “This could help develop better guidelines to prevent unnecessary stenting among the young.”
Touched Off by a Headline
Twitter exploded. “Moronic,” one physician commented. “Criminal,” said another. “Sad and shameful. Misleading to the masses.”
Then Prince Surana, MD, CEO of the Surana Group of Hospitals, chimed in. “I agree the headlines could be misleading,” he tweeted, “but the content of the article is absolutely scientific. We fully stand by it. It was an article and hence the headline and content is not in our control.”
Sripal Bangalore, MD (NYU Langone Medical Center, New York, NY), was one of the cardiologists who stepped into the discussion to point tweeters in the direction of evidence supporting the article’s stance. Interventional cardiologists in India, he tweeted, “have data to show that in very young patients with MI, if the underlying cause is plaque erosion (not rupture) and the lesion is not severe (I assume after aspiration thrombectomy), deferral of stenting is not unreasonable.”
Speaking with TCTMD, Bangalore said he thought many of the cardiologists responding on Twitter “jumped the gun” and started criticizing the paper without understanding the concept of plaque erosion at the heart of the issue.
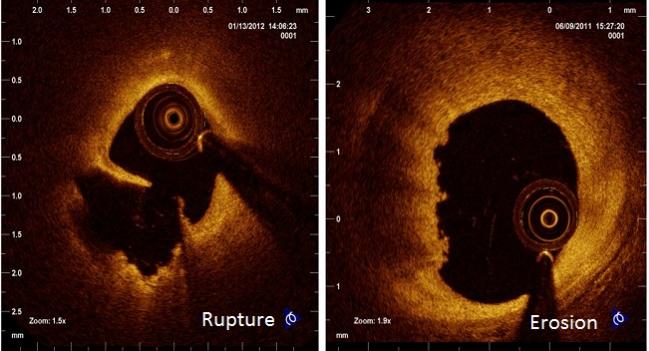
“This has been studied and reported in small observational case series, dating back 20 to 30 years, but now it's becoming more and more important because our imaging techniques have become better,” Bangalore explained. “We can actually now be more precise about plaque erosion without rupture, where there is an intact fibrous cap. What we're referring to is a small group of patients who are pretty young, usually in their 30s . . . with a predominant feature being plaque erosion, not plaque rupture, where there is predominantly clot formation. And the question is, after you aspirate the clot and you're not left with any significant stenosis, can you get away without stenting?”
Not Stenting?
That question was at the heart of the EROSION study, presented as a late-breaker back at the European Society of Cardiology Congress in 2016 and reported at the time by TCTMD. EROSION was a small, single-center, proof-of-concept study of ACS patients in China showing that those screened by OCT and found to have plaque erosion, not rupture, could safely be treated with antithrombotics instead of stenting. At 30 days, 47 out of 60 patients had a more than 50% change in thrombus volume and 22 patients had no residual thrombus; there was no increased risk of recurrent ischemic events. One-year results, subsequently published in Circulation: Cardiovascular Interventions, showed that 92.5% of the 53 patients who’d completed 12-month follow-up and were managed with aspirin and ticagrelor without stenting remained free of major adverse cardiovascular events.
Several experts who spoke with TCTMD suggested that EROSION may have flown under the radar of interventional cardiologists at the time. Many may have dismissed it as a study principally important to Asia, where patients tend to be younger than in North America and Europe and where economic constraints mean that primary PCI with stenting is not always an option.
But Ziad Ali, MD, DPhil (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), who also spoke with TCTMD following the Times of India tweetstorm, believes that physicians are increasingly open to the idea that intracoronary imaging might be more than a research tool, potentially helping to guide treatment strategy. Part of this stems from a growing appreciation of plaque erosion as a distinct entity, making up approximately 25% to 30% of the STEMI cases. Smoking, younger age, female sex, and absence of other CAD risk factors or known CVD are all established predictors of plaque erosion.
But beyond differentiating between eroded versus ruptured plaques, Ali said it’s worth considering whether intravascular imaging, typically used to optimize stent placement, might also prove useful for deciding when a stent may not be necessary—something he stressed has not been studied in large-scale, multicenter, randomized clinical trials.
“The concept is an interesting one and that is, if you have thrombus that’s occluding your artery that can be cleared either by thrombectomy or angioplasty, and you are left with adequate minimal lumen area to provide good flow: in that situation, what is the utility of sort of sealing that plaque rupture with a stent? And the answer to that is completely unknown,” he commented.
Who is going to put a stent and who is going to watch and wait? Ziad Ali
This is particularly important as ACS shifts into younger, previously healthy patients—increasingly the case in countries like India and China, but something also starting to be seen in Europe and North America.
Ali described recently chairing a panel discussion at a cardiology meeting in Australia where he offered the audience a hypothetical scenario. “You have a 50-year-old male patient who has an ACS and you see that the patient has a hazy lesion in the proximal LAD, has a real troponin elevation, and the patient is a few days after his ACS. Now you perform an OCT, you see a plaque rupture, the plaque rupture is empty, there is very minimal residual thrombus, and the minimal lumen area is 5.5 mm2. Who is going to put a stent and who is going to watch and wait?”
He asked for a show of hands: “And it split the room right down the middle.”
In his practice, Bangalore says he is more inclined to use intravascular imaging in younger patients and in women, for whom ruptured plaques are less likely to be the culprit. “If you have a very young patient, in their 20s or 30s, you want to know the underlying mechanism [of their event] before you start throwing in a stent,” Bangalore said. Spontaneous coronary artery dissection (SCAD) is a useful corollary, he said. As recent statements make clear, SCAD—despite having a clinical presentation similar to plaque rupture ACS—has a different mechanism of injury and stenting is not advised in this patient subset. Plaque erosion is yet another phenomenon, with a different etiology, but it may be that here, too, stent implantation is not the right approach, Bangalore mused.
Sticking With the Data
Giulio Guagliumi, MD (ASST Papa Giovanni XXIII, Bergamo, Italy), has been at the forefront of OCT research from its infancy. Speaking with TCTMD, he—like many of the responders on Twitter—expressed concerns that the Times of India article was as much a marketing gambit for the hospital as it was about the theories of plaque erosion and the necessity of stent implantation.
“We need to be very clear about the existing evidence about OCT,” Guagliumi told TCTMD. “OCT is a fascinating technology that has allowed us to do something that in the past was not possible”—namely, get powerful insights into arterial plaques. “But having the data is extremely important,” he stressed. “When we are receiving this type of news we need to stay very close to the data.”
While the theoretical basis for such a strategy is intriguing, “there are multiple caveats in using this technology in these patients,” Guagliumi said. In one out of four patients, he noted, it’s not possible to identify the type of plaque underlying the thrombus, usually because thrombus removal has been ineffective. Also, he continued, any support for such a strategy comes from anecdotal experience or small, single-center series.
“All of the studies we're talking about are observational studies in quite limited numbers of patients or primarily hypothesis-generating studies, he said. “There are absolutely no data from prospective, randomized, multicentered studies.” Even in EROSION, which Guagliumi stressed was conducted by “a very serious group” of investigators, there was no control arm to compare the conservative strategy against current-generation drug-eluting stents.
Moreover, as demonstrated in OCTAVIA, “outcomes following second-generation DES were very, very good,” said Guagliumi, with no differences in vascular response to PCI and stenting between patients identified as having ruptured versus intact plaque at baseline.
Even the cost-efficacy argument (that is, judicious use of OCT may save the upfront and long-term cost of stents), a point emphasized in the Times of India article, falls away in the context of modern-day DES prices in most countries, Guagliumi added.
“Today the price of DES in Europe is absolutely marginal, and the current generation of stents are highly safe—changing the lives of patients who undergo primary PCI,” Guagliumi told TCTMD. So is this kind of conservative approach “feasible and potentially achievable in some patients? The answer seems to be yes,” he continued. But is it also safe and effective? “I don't think we have the answers and when we don't have the answers, we need to be very, very careful in promoting this strategy because . . . there are a lot of potential clinical, logistic, and legal consequences,” Guagliumi cautioned.
He added: “We have to stay in line with the data—otherwise we can destabilize the potential of these technologies.”
And this is a field that doesn’t need destabilization. Worldwide, uptake of intravascular imaging—IVUS, OCT, near-infrared spectroscopy (NIRS)—is patchy at best and tied to reimbursement. In Japan, for example, where it is reimbursed, Ali estimated that intravascular imaging is used in almost 100% of procedures, with OCT accounting for roughly one-third of those tests. In the United States, by contrast, a recent snapshot suggested that intravascular imaging is used in fewer than 5% of PCI procedures, with OCT accounting for around 1% of those procedures. What’s more, OCT use is concentrated in a select number of cath labs. While the vast majority of operators never use OCT, “there are some people in the US who use it 90% to 100% of the time,” Ali said.
Can It Be Studied?
One barrier to studying OCT in the setting of ACS is the concern that the test delays procedures. In capable hands, Ali estimates, OCT prolongs procedural times by 15 minutes, but that doesn’t mean it increases door-to-balloon times, he stressed. “You really need to reestablish flow, and once you've reestablished flow, that's the door-to-balloon or door-to-reperfusion time. And once you've got that, at least the contemporary thought is, you've got time to make other decisions,” such as whether to perform OCT, he explained.
Ali envisions a study where intravascular imaging is used to establish whether an ACS patient has plaque rupture or plaque erosion. If plaque erosion is identified, patients could be treated with thrombectomy or balloon angioplasty. Then, if a minimal lumen area greater than 4.5 mm2 is achieved, they could be randomized to conservative medical therapy versus DES placement.
There’s also a potential role for drug-eluting balloons to be studied in this context, he noted, acknowledging that these devices are not yet approved for coronary interventions in the US and their safety record is currently the subject of an FDA review.
In the meantime, the limited data supporting an OCT-guided, no-stent approach in plaque erosion is coming from China and India, often in collaboration with industry. Certain centers, like Chembur’s Surana Hospital, are already using the technology to guide treatment strategies in this subset of young, previously healthy patients presenting with ACS.
We would use an OCT and not stent the patients if the minimal lesion area is adequate. Mullasari Ajit Sankardas
Mullasari Ajit Sankardas, MD (Madras Medical Mission, Chennai, India), is one of the physicians actively studying outcomes in patients treated with antithrombotics instead of stents. At his institution, he said, he is more likely to use OCT in patients presenting with ACS, calcified lesions, complex lesions, bifurcation lesions, and prior bioresorbable scaffold implantation. In younger patients and smokers, which he points out make up a growing proportion of ACS patients in India, he’s specifically looking for plaque erosion. And in patients with ACS found to have plaque erosion rather than plaque rupture, “We would use an OCT and not stent the patients if the minimal lesion area is adequate,” he told TCTMD.
Sankardas and his co-investigators are working to pull together a two-center data set combining patients from Madras Medical Mission and Lisie Hospital in Kochi, India, to track outcomes in patients identified as having plaque erosion and treated conservatively without stenting. The project is being conducted in collaboration with Massachusetts General Hospital, he said.
To date, however, published data are scant. “At the end of the day,” Bangalore said, “the trialists will say we need a randomized trial, and I can tell you, yes, from a purist’s point of view, we do. But I don't think it's feasible at all given that this is a relatively rare group and it’s not easy to find them.”
Chinese investigators, meanwhile, are moving forward with EROSION II. The nonrandomized, multicenter study kicked off in 2017 with the aim of enrolling 340 patients with STEMI < 12 hours and identified as having plaque rupture or erosion on OCT without obstructive stenosis (diameter stenosis < 70%) to see whether patients can be stabilized by effective antithrombotic treatment without stent implantation, thereby avoiding both early and late complications related to PCI.
The primary endpoint is reduction in thrombus burden on OCT at 30 days, and the secondary outcomes include a comparison of major adverse cardiovascular events among patients identified as having rupture versus thrombus out to 1 year.
Next Steps
For now, most interventionalists continue to view intracoronary imaging—be it IVUS, OCT, or NIRS—as a research frill, not something they could use on a more routine basis to guide clinical decision-making. Guagliumi and colleagues hope to clear up some of the confusion with a consensus document that will be released at the upcoming EuroPCR meeting. Thomas Johnson, MD (Bristol Heart Institute, UK) will presented the document in a keynote lecture entitled "Clinical Use of Intracoronary Imaging on the opening day of the meeting."
Biased and sensational headlines can confuse even fairly educated patients and sometimes can lead to mistrust in the physician, delaying the standard-of-care treatment. Purvi Parwani
Ali and Bangalore, for their part, hope that the Twitter melee prompted some interventionalists to step back and consider the knowns and unknowns about the necessity of stenting in certain patient subsets. For Ali, that group is specifically patients presenting with ACS in whom an adequate lumen area can be achieved through balloon dilation, thrombectomy, or thrombolysis. “There are now emerging data sets to show that treatment of these patients with thrombectomy followed by dual antiplatelet therapy, and in some situations anticoagulation with warfarin, leads to complete resolution of the thrombus and complete healing of the artery wall,” Ali said.
“Theoretically, it's a very interesting concept,” he added. “While I think the [Times of India] article was written in a provocative way, the concept has utility, there's no question.”
Parwani, for her part, said she “learned a lot from the discussion” her tweet sparked. And she’s intrigued by the potential for OCT, if properly studied, to provide additional insights into appropriate care, especially for these younger MI patients. “There’s lots of opportunities to investigate this further,” she said.
This doesn’t detract from the fact that headlines like these can have a broader impact, stressed Parwani, who specializes in cardiac imaging and preventive cardiology. This is particularly true for a country like India where so few people can afford the standard of care offered in countries like the US, where she practices, and are therefore potentially more susceptible to misleading media reports.
Her own family, which includes a number of physicians, called her after seeing the Times of India article, one asking her if he’d even needed the stent he’d received previously, Parwani noted.
“Biased and sensational headlines can confuse even fairly educated patients and sometimes can lead to mistrust in the physician, delaying the standard-of-care treatment,” she insisted. “This is particularly applicable in India where patients pay out of pocket and hence whenever you use a certain technology or equipment you have to speak with them and make sure they will agree to pay. They also have the power to refuse the treatment, and I fear you may see some patients who do need the standard of care not get it because of that.”
Photo Credit: Jang I-K. Diagnosis and treatment of erosion in ACS: The EROSION study. Presented at: TCT 2016. November 1, 2016. Washington, DC.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioDisclosures
- Ali reports serving on the scientific advisory board of and receiving honoraria from Abbott, and serving as principal investigator for the Abbott-sponsored ILUMIEN IV trial.
- Guagliumi reports receiving grants and personal fees from Boston Scientific and Abbott.
- Parwani and Bangalore report no relevant conflicts of interest.


Comments