OCT, IVUS Each Boost Long-term Outcomes When Used to Guide PCI, Study Suggests
Both intravascular tools fared better than standalone angiography but are seldom used around the globe, in part due to time and cost.
Outcomes from PCI are better when some type of intravascular imaging—either optical coherence tomography (OCT) or IVUS—are used to guide the procedure, suggest findings from a registry study.
Compared with angiographic guidance alone, use of either OCT or IVUS was associated with better procedural success and in-hospital outcomes and lower long-term mortality, with differences observed in both elective and ACS cohorts, researchers led by Daniel Jones, MD, PhD (St. Bartholomew’s Hospital, London, England), report in a study published online ahead of the July 23, 2018, issue of JACC: Cardiovascular Interventions.
“Importantly, we believe this for the first time provides an answer to the debate about the role of invasive imaging in guiding PCI, showing that both IVUS and OCT outperform standalone angiography and are equally effective in improving short- and long-term outcomes,” Jones told TCTMD in an email.
“This analysis and emerging data from randomized controlled studies are expected to broaden the use of intravascular imaging in guiding PCI,” he added.
Ziad Ali, MD, DPhil (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), who was not involved in the study, said it “confirms all of the things that we’ve already seen with intravascular imaging, but now for the first time, also showing it as a benefit for OCT.”
There are limitations to observational studies like this one, and selection bias cannot be completely ameliorated even with sophisticated statistical adjustment like that used in this study, he pointed out. That bias might explain some of the benefits attributed to OCT.
What the study does “is put us in a position of strength to push forward with a large randomized controlled trial, which we’re conducting in ILUMIEN IV,” to confirm the benefits OCT versus angiographic guidance, Ali said. The trial, which has just begun randomizing patients to angiographic guidance or OCT guidance with a specific stent-sizing algorithm, is enrolling only complex and high-risk patients because it is in that type of population that OCT guidance would be expected to have the most benefit, he explained.
“It’s not that there wouldn’t be a benefit as is shown in the current registry in all patients, but the number needed to treat in order to achieve that benefit might be outside the scope of everyday practice,” Ali said. “Really what we need to do is focus on which patients are most likely to benefit in these really cost-driven times.”
In light of the findings of this new study, “we should all be enthusiastic about enrolling in the randomized controlled trial to show that this is not an effect of confounders but rather it’s a real effect of imaging guidance versus angiography guidance,” he said.
Shortcomings of Angiography
Angiography has limitations when it comes to assessing luminal dimensions, vessel wall pathology, and results of stenting, the authors explain. IVUS and OCT can add to what can be gleaned from angiography, with the former being the more mature technology. Although there are some data suggesting clinical benefits from using OCT—including from the ILUMIEN I, ILUMIEN II, ILUMIEN III: OPTIMIZE PCI, and DOCTORS studies—there is limited information on its effects on clinical endpoints, particularly over the long term.
In the current study, Jones et al turned to the Pan-London PCI registry cohort, which includes patients who underwent PCI at nine London-area primary PCI centers between January 2005 and May 2015. This analysis excluded those undergoing primary PCI for STEMI or who had pressure wires used during their procedure, leaving 87,166 patients followed for a median of 4.8 years.
OCT was used in 1.3% of patients, IVUS in 12.6%, and angiography alone in the rest. Rates of both OCT and IVUS increased over time, with significant variation across centers.
Procedural success rates were higher with OCT (97.7%) and IVUS (95.7%) than with angiography alone (94.3%). Mean stent length increased from the angiography group (21.0 mm) to the IVUS group (23.5 mm) to the OCT group (25.8 mm). Procedural complications occurred at similar rates across all three groups.
In the hospital, MACE rates were lower with OCT (1.3%) and IVUS (1.4%) than with angiography (1.8%), driven mostly by lower rates of death and recurrent MI.
That difference in mortality was maintained during follow-up, with unadjusted MACE rates of 7.7% in the OCT group, 12.2% in the IVUS group, and 15.7% in the angiography group (P < 0.0001). After adjustment, the risk of long-term mortality was lower with both OCT (HR 0.48; 95% CI 0.26-0.81) and IVUS (HR 0.72; 95% CI 0.32-0.93) when compared with angiography. After propensity-score matching, there was no difference in mortality between the OCT and IVUS groups.
Pooling the OCT and IVUS groups together, intravascular imaging was associated with lower risks of in-hospital MACE and long-term mortality.
OCT or IVUS?
When asked about choosing between OCT and IVUS, Ali responded: “Overall, from the interventional population point of view, it’s important to be familiar with both, but I think it’s really a class effect rather than a specific effect. I think the use of intravascular imaging in general, whether it be OCT or IVUS, provides a benefit as was shown in this study. But like many things, you need the right tool dependent upon the job and you pick the tool dependent upon what you’re trying to find out.”
I think the use of intravascular imaging in general, whether it be OCT or IVUS, provides a benefit as was shown in this study. Ziad Ali
The key reasons for using intravascular imaging—to determine normal segments of the artery in which to land a stent, to choose to appropriate stent size, to make sure the stent is fully expanded, and to ensure that there are no post-PCI complications either at the edge or within the stent—can be achieved by either modality, he explained. Also, the costs of OCT and IVUS are similar, and both are reimbursed, he added.
Although OCT has some software features that automate the procedure, anything that can be identified on OCT can also be identified by IVUS, he said. “The key component here is to increase the utilization of intravascular imaging and familiarize people with how it’s likely to benefit patients.”
Indeed, there has been some resistance to incorporating intravascular imaging on the part of many operators, as noted in an accompanying editorial by Carlo Di Mario, MD, PhD, and Alessio Mattesini, MD (Careggi University Hospital, Florence, Italy).
“There is a lower overall rate of use of intravascular imaging globally than in the nine participating cardiac centers across London, with the exception of Japan, Korea, and in part, the United States,” they write. “Time and cost are the most frequent reasons put forward to justify this reduced use but the real explanations are more fundamental questions on the efficacy of IVUS/OCT to improve outcome. Many expert interventional cardiologists suggest that intravascular imaging is good only in a learning phase, but once you have learned how to use a new device or practiced the technique to treat a complex bifurcational lesion, you can skip doing intravascular imaging and simply rely on angiography.
“Despite the better outcome of this very large registry in the imaging group,” they say, “it is unlikely that this study will overcome these resistances.”
More data are therefore needed to confirm the benefits of OCT-guided PCI, but while the community awaits the results of ILUMIEN IV and OCTOBER, Di Mario and Mattesini say, “the indications of the most recent guidelines push even the sceptics to a more liberal use of these imaging techniques.”
Jones agreed that further research is needed “to identify the group of patients and lesion types in which OCT guidance during PCI is associated with net prognostic benefit.”
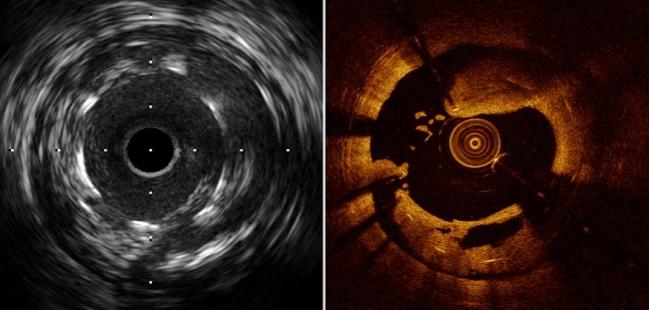
Photo Credit: Guagliumi G. State-of-the-art review: intravascular imaging and physiology to evaluate stent thrombosis and restenosis. Presented at: TCT 2017. November 1, 2017. Denver, CO.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Jones DA, Rathod KS, Koganti S, et al. Angiography alone versus angiography plus optical coherence tomography to guide percutaneous coronary intervention: outcomes from the Pan-London PCI cohort. J Am Coll Cardiol Intv. 2018;11:1313-1321.
Di Mario C, Mattesini A. Will optical coherence tomography become the standard imaging tool for percutaneous coronary intervention guidance? J Am Coll Cardiol Intv. 2018;11:1322-1324.
Disclosures
- Jones, Di Mario, and Mattesini report no relevant conflicts of interest.


Comments