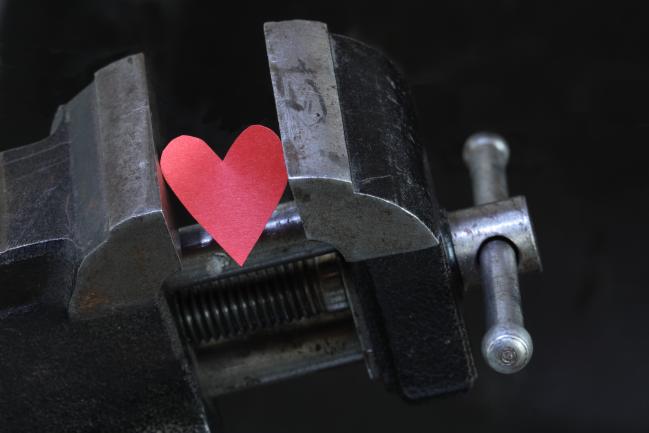
Once Again, ISCHEMIA Trial Feels the Squeeze
There’s more hand-wringing, and more controversy, as the ISCHEMIA design paper sees the light of day. Will PCI or OMT win out in stable, ischemic CAD?
In a sign of just how much attention is being paid to the $100 million ISCHEMIA trial, two experts have published a perspective accompanying what is normally a cut-and-dried paper on trial design, suggesting that the trial may not answer critical questions concerning the best treatment option for patients with stable ischemic heart disease.
Venkatesh Murthy, MD, and Kim Eagle, MD (University of Michigan, Ann Arbor), make the case that changing the primary endpoint to include softer clinical events, such as hospitalization for heart failure and angina, as well as including patients with less ischemic burden, may hinder its applicability when the results are finally known in 2019 or 2020.
“ISCHEMIA may have enough heterogeneity in the way people can interpret it, where even after we’ve spent untold millions on the study, we might not have an answer,” Murthy told TCTMD.
This isn’t the first time this concern has been raised. Trial investigators recently drew the ire of the cardiology community when the primary endpoint was expanded from cardiovascular death and MI to include resuscitated cardiac arrest, hospitalization for unstable angina, and hospitalization for heart failure.
The National Heart, Lung, and Blood Institute (NHLBI)-sponsored study is comparing an initial invasive strategy with PCI or CABG plus optimal medical therapy against a conservative treatment strategy of medical therapy alone in stable patients with moderate-to-severe ischemia on stress testing.
For some, the trial was weakened in its modification to include more subjective endpoints, while investigators argued they had to be realistic given slow enrollment and lower-than-anticipated event rates.
For William Boden, MD (VA New England Healthcare System, Boston, MA), one of ISCHEMIA’s principal investigators, the criticisms are inevitable. He told TCTMD that this is only the start of the debate surrounding trial design, the selection of endpoints, and later on, its outcomes. “This is just the beginning,” he said. “It’s not a tempest in a teapot. It’s something people are going to chew on for some time to come.”
Defining ISCHEMIA and Other Concerns
While the prespecified changes to the primary endpoint have attracted the most attention to date—and even led to a controversial back-and-forth in Circulation: Cardiovascular Quality and Outcomes—Murthy said he’s most concerned about the definition of ischemia in the trial.
In their perspective, which was originally published online June 20, 2018, in the American Heart Journal, Murthy and Eagle point out that the ISCHEMIA investigators initially insisted only on stress imaging tests with rigorous core lab adjudication of ischemia burden prior to randomization. Only patients who demonstrated more than 10% ischemia on nuclear perfusion imaging were eligible for enrollment, but the trial has since been expanded to include patients with only 5% ischemic burden at low levels of exertion (≤ 7 METS). Additionally, the trial now includes patients with ECG changes during exercise testing without imaging.
Murthy told TCTMD that if ISCHEMIA is negative—that is, if coronary revascularization is shown to be no better than optimal medical therapy—interventional cardiologists might be reluctant to apply the results to their practice. They could argue, for example, that their patients are sicker and have greater ischemic burden than the patients enrolled in the trial.
As for enrolling patients with ischemia assessed with a treadmill ECG, Murthy said ECG findings without imaging can be tough to assess, with the results varying by gender, obesity status, and many other factors. Also, the association between ST-segment depression on exercise ECG and ischemia on stress testing is poor, and the algorithm used by the ISCHEMIA investigators hasn’t been validated, he said.
“When you have a diverse collection of patients who get into the study in a variety of ways, regardless of whether you have a positive or negative trial, the change in inclusion criteria is going to be tough in terms of applying the study results,” said Murthy.
In their perspective, Murthy and Eagle also point out that ISCHEMIA is a global trial and practice patterns and patient preference vary from country to country. Being part of a randomized trial where stents are free has the potential to impact the study results, particularly in countries where the cost of DES remains very high, they argued.
No Surprises Here
To TCTMD, Boden said the perspective raises valid points that have come up in discussions with other physicians, both on social media and at medical meetings. The original plan was to enroll 8,000 patients with stable coronary heart disease and severe ischemia—those with 10% or greater ischemic burden of the left ventricle—but along the way investigators had to make concessions.
A number of factors led to the practical decision to lessen the amount of ischemia that would otherwise let patients into the trial. Given the funding from the NHLBI, they had to meet various enrollment milestones and could not get too far behind. Additionally, physician behavior and current practice patterns also made enrollment a challenge. Boden said that because physicians did not know the coronary anatomy of patients prior to randomization, they were cautious in randomizing patients to one of the two treatment arms.
“I think cardiologists instinctively rely on knowing the anatomy,” he said. “If you don’t know the anatomy, and you’re confronted with a patient who has ischemia in 10% of the left ventricle, you run the risk that those patients are not going to get into the trial because the cardiologist is rightly concerned they may be deprived of the benefit of revascularization in that setting.”
As for the use of ECG testing, Boden said myocardial imaging is less commonly used in Europe, where they more frequently rely on standard treadmill exercise testing as the noninvasive diagnostic test for ischemia. Making this modification also made it easier for the ISCHEMIA investigators to complete trial enrollment, which reached 5,179 patients.
Changes in the Primary Endpoint
Murthy and Eagle suggest it’s possible some bias has been introduced into ISCHEMIA, noting that “faith healing” and “subtraction anxiety” could have an impact on the softer clinical endpoints.
“These are very experienced investigators and they did as good a job [as possible] in setting the endpoint definitions,” said Murthy. “The real question comes down to the doctor’s themselves. For example, knowing that a patient had a coronary revascularization—not the trial doctor now, but the doctor on the ground, managing the patient—they are more likely to tell the patient their atypical symptom is nothing to worry about and you don’t need to go into the emergency department.”
With the phenomenon of faith healing, despite the most rigorous definitions of MI, trial leaders can’t assess what’s never been evaluated, said Murthy. On the flip side, with subtraction anxiety, if the physician knows their patient hasn’t undergone PCI or bypass surgery, they might be more likely to tell the patient to head to the emergency department when atypical symptoms present.
Faith healing and subtraction anxiety—both of which potentially introduce bias into studies that use softer endpoints, such as hospitalization for heart failure and angina—are issues physicians are talking about more and more following the ORBITA trial, where PCI was shown to be associated with a placebo effect. Over the 6-week study, those who underwent PCI for stable, single-vessel disease fared no better than individuals treated with a sham procedure when it came to an improvement in exercise capacity and angina symptoms.
ORBITA and Sham-Controlled Trials
Boden told TCTMD that it’s unfair to criticize ISCHEMIA—a study designed in 2011—based on findings from ORBITA. At the time, nobody was thinking about sham-controlled PCI trials, he said.
That said, faith healing and subtraction anxiety are important factors, particularly if you have a softer endpoint. Even the NHLBI was firm in having a hard endpoint of cardiovascular death and MI when the ISCHEMIA trial was designed. However, knowing that even the best-laid plans of clinical trials sometimes fall through, the trial protocol allowed researchers to modify the endpoint according to prespecified rules if enrollment was slow or the event rate was lower than expected.
Even though the decision to develop a prespecified contingency plan is valid and proper, Boden acknowledges that it opens the group up to criticism. “Whether prespecified or not, people are going to recall that it was initially planned to assess cardiovascular death and MI,” he said. “It’s an inescapable criticism.”
Despite these concerns, Murthy praised the ISCHEMIA investigators for investing their time and energy to conduct the $100 million trial. The study will help clinicians understand the fundamental question of how much ischemia matters when it comes to deciding on the optimal treatment strategy for patients with stable coronary heart disease.
Going forward, Murthy and Eagle suggest in their perspective that one way to mitigate controversy will be to maximize openness and disclosure of trial resources and data. The public release of detailed operating procedures, core lab protocols, data safety monitoring board protocols, and statistical analysis plans would help serve to underscore the integrity of the trial, they suggest.
When Perspective Courts Controversy
Adding further intrigue to an already snarled story, the editorial by Murthy and Eagle was briefly taken down and republished online this week amid concerns there were errors in the prepublication copy, according to American Heart Journal editor-in-chief Daniel Mark, MD (Duke University Medical Center, Durham, NC).
The removal didn’t go unnoticed and raised eyebrows on #CardioTwitter. One physician tweeted that the paper’s disappearance represented “DEEPLY CONCERNING editorial behavior.” Others said it smacks of censorship.
Responding on Twitter, Mark, who is also an ISCHEMIA investigator, initially said “the commentary is under minor revision and will be back online when authors are finished with it.” However, the uncorrected version reappeared online following the outcry on Twitter and is still available. Mark tweeted that the perspective is currently slated for the September print issue and “the revision process does not affect its status in any way.”
In fact, Mark told TCTMD in an email that they have already received the corrected perspective and the updated version should be “available online within a day and will be available going forward.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Murthy VL, Eagle KA. ISCHEMIA: a search for clarity and why we may not find it. Am Heart J. 2018;Epub ahead of print.
Disclosures
- Murthy reports owning stock in General Electric, Medtronic, Johnson & Johnson, Amgen, and Cardinal Health; receiving consulting fees and research grants from and serving on the advisory board for Ionetix; receiving research grants from Siemens Medical Imaging; and being supported by the NHLBI.


Comments