Operator, Hospital Experience Matter for CTO PCI Success
The findings support centralization of CTO PCI in highly experienced centers—that might be tricky in the US.
Patients with chronic total occlusion (CTO) have better outcomes when their PCI is performed by operators who more frequently do these complex cases and when it’s done at experienced centers, data from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) show.
Both operator and hospital experience seem to make a difference in terms of procedural success and in-hospital mortality, researchers led by Rami Zein, DO (Ascension St. John Hospital, Detroit, MI), report in a study recently published online in Circulation: Cardiovascular Interventions.
Much prior CTO PCI research has come from dedicated registries involving the most-expert operators and centers, where success rates of 80% to 90% have been reported, senior author Hitinder Gurm, MBBS (University of Michigan, Ann Arbor), told TCTMD. That likely doesn’t reflect what’s happening out in the broader community, a scenario explored in the current study.
It’s “not a surprise that the more CTOs you’ve done, the better your outcomes are, but what probably was more surprising was how few CTOs most operators are doing or have done,” Gurm said. Across Michigan, operators had performed a median of 12 CTO PCIs in their careers, with 8.9% having performed more than 50. Only 8.7% of centers had performed more than 50 such procedures per year.
“I think it’s a just an honest reflection of what is happening in the community,” Gurm said, “and what happens in Michigan is probably a pretty reasonable approximation of what happens across the United States.”
The investigators and other commentators said the study supports regionalization of CTO care, such that CTO PCI is concentrated in the most-experienced hands, although challenges were seen to implementing that approach in the United States.
BMC2 Registry
Using the BMC2 quality-improvement registry, Zein, Gurm, and colleagues examined data on 7,389 patients in whom CTO PCI was attempted at 46 sites across Michigan between January 2010 and March 2018. The overall rate of procedural success, defined as < 50% angiographic stenosis with TIMI grade 3 flow after the procedure without any MACE (death, urgent CABG, stroke, or tamponade), was just 53%.
Operators were divided into tertiles based on their lifetime experience with CTO PCI—less than 12, 12 to 33, or more than 33 cases. The procedural success rate increased across the three groups, from 45% to 65%, with a similar trend for hospital experience. The best procedural success was achieved by the most-expert operators at centers with the highest experience, whereas the worst was obtained by inexperienced operators at centers with the least experience.
In the periprocedural period, CTO PCI performed by operators with the most experience was associated with higher rates of cardiac tamponade, major bleeding, transfusion, MI, cardiogenic shock, and stroke. The researchers attribute that to both the higher risk level of the patients treated by the most-expert operators and the use of more-aggressive procedural techniques, which may result in coronary perforation.
“However, the fact that more-experienced operators had less emergent open-heart surgeries, repeat PCIs, as well as the lowest length of hospital stay and lower risk-adjusted mortality suggests that these complications were managed expeditiously and more effectively by these operators, perhaps accounting for lower in-hospital death rates despite higher MACE rates,” Zein et al write in their paper.
Multivariable logistic regression models showed that prior operator and site experience was positively associated with procedural success (P < 0.001), but not MACE (P = 0.208).
Regionalization of CTO PCI
Commenting for TCTMD, Tim Kinnaird, MD (University Hospital of Wales, Cardiff), said the study’s findings resonate with work being done by his research group using British Cardiovascular Intervention Society data. Prior studies have not necessarily shown that procedure experience has a big impact on outcomes of general PCI, but “certainly as you crank up the complexity—with CTO being the most complex of all coronary interventions—then I think most of us that do CTO and do complex PCI believe that practice does make perfect.”
What struck him about these new data, Kinnaird noted, were the low numbers of CTO PCI procedures performed by most operators and the relatively low success rates even in the most experienced hands. “We know from CTO registries that you can achieve 90% success rates,” he said, noting that that was achieved at his center after the CTO pathway was revamped.
The key, according to Kinnaird, is to get patients to the right operators for treatment. “CTO PCI should be done by CTO specialists. I don’t think there’s any doubt about that. All of the data support that,” he said. “And I believe that physicians should get over themselves a little and just put the patient at the forefront. I’m not always convinced that’s the case. I may be being slightly controversial now, but there are obviously financial disincentives to referral. There’s a lack of awareness of success rates. I guess there’s egos in the way, as well. So there’s lots of reasons that patients aren’t referred to the right person.”
The study authors agree in principal with a more-regionalized approach to care. “We believe that in the ideal world, CTO PCI should only be performed by a highly experienced operator at a highly experienced center with careful assessment of risk and benefit,” Zein and Gurm said in an email. But, they pointed out, “there are significant policy, business, and practice barriers that are likely to prevent such regionalization. We have seen this with other procedures, and while such regionalization is ideal, it is unlikely to happen in the near future given lack of any pressure to the contrary.”
Gurm said in an interview that “our hope is to start that dialog” around regionalization. “Hopefully there’ll be some discussion as to how we can get to that point.”
Other Options
Centralizing care in a few select centers might not be the only way to improve the success of CTO PCI, Gurm proposed, highlighting the finding that among the operators with the least experience, those practicing at highly experienced centers achieved better outcomes than those practicing at hospitals with less experience.
“It may be that if you get mentoring and proctoring and guidance from someone who’s more experienced, that would lead to better outcomes at the hands of the less-experienced operators,” Gurm said. “Most of those less-experienced operators are working at less-experienced sites. We’re trying to come up with some kind of learning-network approach . . . to see how can the more-experienced operators provide guidance to less-experienced operators who are not at their center or not part of the network.” Such an initiative, currently being explored by the BMC2 in Michigan, would provide operators with feedback on the procedures they’re doing as well as advice on the kinds of cases that they should be referring to more-experienced interventionalists, Gurm said.
Along those lines, Prashant Kaul, MD, and David Kandzari, MD (both Piedmont Heart Institute, Atlanta, GA), write in an accompanying editorial: “Notwithstanding the ongoing discussion regarding indications and appropriateness of CTO revascularization, results of the present study should encourage professional societies and the CTO community to address the training for and performance of CTO PCI procedures.
“Aside from best practice sharing, efforts to standardize procedural strategy (and therefore minimize human variability), and enhancing skill sets and preparedness, advancement of CTO PCI is in need of oversight and policy,” they continue. “In the patient’s best interest for likelihood of initial success, rather than encourage performance by antegrade-only operators, CTO interventionalists should demonstrate competency for antegrade, retrograde, and dissection/re-entry methods. Although what constitutes a minimum case volume to establish proficiency (and independent practice) may be contested, more important will be ongoing program surveillance with performance metrics and quality assessment.”
The discussion about possible ways to regionalize CTO PCI and improve patient outcomes is still in the early stages, Zein noted to TCTMD. “We’re still in the infancy of trying to standardize who does them and where we do them. But I think it’s a work in progress and hopefully as CTO PCI, and high-risk PCI for that matter, become more mainstream and operators start to know what they want to do or what their limitations are, [we can start to] refer out or to find the best operators for these cases or for these patients.”
Patients considering CTO PCI might help drive the centralization of care, Gurm suggested. “They should be willing to have that dialog with their physician as to their experience and outcome, and I think that will help automatically lead to some regionalization and specialization.”
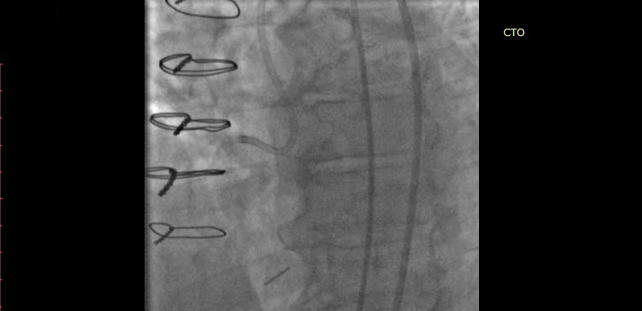
Photo Credit: Pershad A. Case selection for CTO PCI: case examples. Presented at: CTO 2020. February 20, 2020. New York, NY.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Zein R, Seth M, Othman H, et al. Association of operator and hospital experience with procedural success rates and outcomes in patients undergoing percutaneous coronary interventions for chronic total occlusions. Circ Cardiovasc Interv. 2020;13:e008863.
Kaul P, Kandzari DE. Chronic total occlusions: practice makes perfect—implications for standardizing performance and training. Circ Cardiovasc Interv. 2020;13:e009724.
Disclosures
- The study was supported by the Blue Cross Blue Shield of Michigan and Blue Care Network as part of the Blue Cross Blue Shield of Michigan Value Partnerships program.
- Zein reports no relevant conflicts of interest.
- Gurm reports being a consultant to Osprey Medical and receiving research funding from the US National Institutes of Health’s Centers for Accelerated Innovations and Blue Cross Blue Shield of Michigan.
- Kaul reports having received honoraria for consulting fees from Abbott Vascular, Boston Scientific, Cardiovascular Systems Inc, and Philips.
- Kandzari reports having received personal consulting honoraria from Abbott Vascular, Biotronik, Cardiovascular Systems Inc, and Medtronic; and institutional research grant support from Abbott Vascular, Biotronik, Boston Scientific, Cardiovascular Systems Inc, Orbus Neich, Medtronic, and Teleflex.


Comments