Oral PCSK9 Inhibitor Reduces LDL Cholesterol in Phase IIb Study
The drug, MK-0616, was effective and well tolerated in patients with a variety of ASCVD risks. Phase III plans are now afoot.
NEW ORLEANS, LA—An investigational oral PCSK9 inhibitor has shown promise for patients with hypercholesterolemia with a range of atherosclerotic cardiovascular disease (ASCVD) risks in a phase IIb trial.
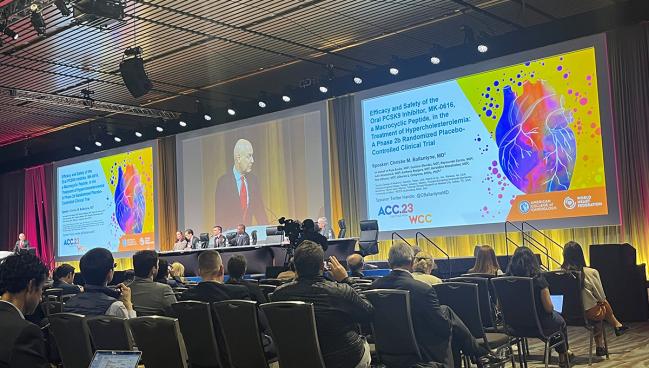
The drug candidate, dubbed MK-0616, provided reductions in LDL cholesterol of up to 60.9% relative to placebo through 8 weeks of treatment, with significant reductions in apolipoprotein B (apoB) and non-HDL cholesterol as well, Christie Ballantyne, MD (Baylor College of Medicine, Houston, TX), reported here at the American College of Cardiology/World Congress of Cardiology (ACC/WCC) 2023 meeting. The drug was well tolerated.
The data, published simultaneously online in the Journal of the American College of Cardiology, “support the further development of MK-0616, an oral PCSK9 inhibitor that may improve access to effective LDL cholesterol-lowering therapies and improve attainment of guideline-recommended LDL goals aimed at reducing cardiovascular risk,” Ballantyne concluded. A phase III program is currently being designed, he added.
Though injectable PCSK9 inhibitors provide large reductions in LDL cholesterol, and have been shown to reduce ASCVD events, their adoption has been limited by access issues and perhaps by the need for repeat injections. It’s possible, Ballantyne suggested, that an oral PCSK9 inhibitor may improve uptake and thus the attainment of guideline-recommended treatment goals.
An oral option is definitely going to be really important in terms of getting patients on appropriate therapy to achieve LDL goals and reduce ASCVD risk. Dave Dixon
Phase I data on MK-0616, a macrocyclic peptide with 1/100th of the molecular weight of the injectable monoclonal antibodies, showed large reductions in LDL cholesterol on top of statin therapy and a lack of serious adverse events.
To explore the drug further in phase IIb, investigators randomized 381 patients (mean age 61.5 years; 49.3% women) with hypercholesterolemia to placebo or one of four doses of MK-0616—6, 12, 18, or 30 mg once daily. Most patients (56.4%) had intermediate-to-high risk of ASCVD, 38.6% had clinical ASCVD, and 4.7% had borderline ASCVD risk.
In terms of background lipid-lowering therapy, roughly 40% of participants were not taking statins, about one-third were on moderate-intensity statin therapy, and about one-quarter were on high-intensity statin therapy. Mean LDL cholesterol at baseline was 119.5 mg/dL.
The primary endpoint was the change in LDL cholesterol after 8 weeks of treatment, with observed reductions relative to placebo ranging from 41.2% with the 6-mg dose of MK-0616 to 60.9% with the 30-mg dose (P < 0.001 for all). Nearly all of the efficacy was achieved in the first 2 weeks and then sustained through the end of the treatment period.
Reductions in apoB and non-HDL cholesterol were of similar magnitude.
Protocol-defined LDL-cholesterol goals varied based on background ASCVD risk—less than 70 mg/dL for those with clinical ASCVD, less than 100 mg/dL for those with intermediate-to-high risk of ASCVD, and less than 130 for those with borderline ASCVD risk. These goals were achieved by 80.5%, 85.5%, 90.8%, and 90.8% of patients in the four increasing MK-0616 dose groups, respectively, compared with 9.3% in the placebo group.
The drug was well tolerated, Ballantyne reported, with an overall adverse event rate of 44.0% in the placebo group and rates of 39.5% to 44.2% across the drug groups. There was one death in the study, but it was deemed unrelated to treatment (motor vehicle accident).
Potential for More Options for Patients
Commenting for TCTMD, Dave Dixon, PharmD (Virginia Commonwealth University, Richmond), a member of the ACC Prevention of Cardiovascular Disease Council, explained why an oral option for PCSK9 inhibition would be welcome if it eventually comes to market.
“Injectable therapies can be met with some resistance . . . and in some cases, self-injection is either not desirable or not feasible—for example, if someone has a tremor disorder or severe arthritis,” he said. “So an oral option is definitely going to be really important in terms of getting patients on appropriate therapy to achieve LDL goals and reduce ASCVD risk.”
New therapies typically come with a high cost, which was—at least initially—one of the main barriers to uptake of the injectable PCSK9 inhibitors. If this oral PCSK9 inhibitor eventually gets regulatory approval, “I think it will be imperative that the manufacturer of this product take that into consideration and ideally come in at a price point that will help ensure patient access,” Dixon said. “Because right now that’s really one of the primary barriers we have to getting patients on effective preventive therapies, treating LDL appropriately, and ultimately being able to bend the curve on cardiovascular disease in this country.”
I think the future is bright for LDL-lowering and atherosclerosis in our patients, and we are now really chipping away at the barriers to achieving that holy grail. Rhonda Cooper-DeHoff
Dixon said that at this point, he doesn’t have any specific safety concerns with MK-0616, noting that like the monoclonal antibodies that inhibit PCSK9, this molecule appears to be too big to cross the blood-brain barrier. “That does give me some hope from the standpoint of at least reducing the likelihood of any neurocognitive effects,” he said.
Larger studies of the drug will be needed, however, to fully understand the safety profile, said Dixon.
Still, he had a positive view of the long-term prospects of MK-0616. “Anytime that we can have an oral option for patients, I think that’s great,” he said. “I do think it will be interesting to see how this plays out in the long run, especially now that we have inclisiran on the market, which is a twice-yearly injection.” Some patients, he said, are fine taking a pill every day, others prefer self-injections, and still others might prefer less-frequent drug administration, which they would get with inclisiran.
“At the end of the day, it’s all about giving the patient options, and so this is really encouraging data to see here,” Dixon said.
Speaking at a news conference, Rhonda Cooper-DeHoff, PharmD (University of Florida, Gainesville), a member of the ACC CV Team Pharmacists Work Group, also welcomed the potential for new treatment options, pointing both to the current study and to the CLEAR Outcomes study of bempedoic acid (Nexletol; Esperion) presented earlier in the meeting.
“I think the future is bright for LDL-lowering and atherosclerosis in our patients, and we are now really chipping away at the barriers to achieving that holy grail for our patients—that is, guideline-directed LDL-lowering to prevent hard outcomes,” she said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Ballantyne CM, Banka P, Mendez G, et al. Efficacy and safety of the oral PCSK9 inhibitor MK-0616: a phase 2b randomized controlled trial. J Am Coll Cardiol. 2023;Epub ahead of print.
Disclosures
- Merck Sharp & Dohme LLC, a subsidiary of Merck & Co, funded the study.
- Ballantyne reports having received grant/research support through his institution from Abbott Diagnostics, Akcea, Amgen, Arrowhead, Esperion, Ionis, Merck, New Amsterdam, Novartis, Novo Nordisk, Regeneron, and Roche Diagnostics and having been a consultant for 89Bio, Abbott Diagnostics, Alnylam Pharmaceuticals, Althera, Amarin, Amgen, Arrowhead, AstraZeneca, Denka Seiken, Esperion, Genentech, Gilead, Illumina, Ionis, Matinas BioPharma Inc, Merck, New Amsterdam, Novartis, Novo Nordisk, Pfizer, Regeneron, and Roche Diagnostics.





Comments