Polypill Bests Usual Care in Patients With Recent MI: SECURE
Now with a “striking” win in secondary prevention, experts believe it’s time to more broadly adopt this simple strategy.

BARCELONA, Spain—(UPDATED) The use of a polypill that contains aspirin, an ACE inhibitor, and a statin significantly slashes the risk of major cardiovascular events when compared with usual care in elderly patients who have recently had a myocardial infarction, according to a new randomized study presented today at the European Society of Cardiology (ESC) Congress 2022.
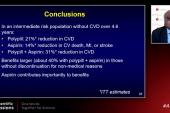
In SECURE, the polypill strategy reduced the risk of cardiovascular death, nonfatal MI, nonfatal ischemic stroke, or urgent revascularization, the study’s primary endpoint, by 24% compared with a strategy where patients took guideline-directed medications individually. With respect to the harder endpoint of cardiovascular death, nonfatal MI, and nonfatal stroke, use of the polypill reduced the risk by 30% compared with usual care.
Principal investigator Valentin Fuster, MD (Icahn School of Medicine at Mount Sinai, New York/Centro Nacional de Investigaciones Cardiovasculares, Madrid, Spain), likened the polypill’s success in SECURE to some of the landmark studies showing aspirin’s benefit in secondary prevention or the first big statin trials in patients with coronary heart disease.
“The curves begin to separate from the very beginning of the trial, and they continue to separate,” Fuster told the media during an ESC press conference. “One can begin to project the possibility that the results will be even more striking if the trial continues follow-up.”
The polypill is a straightforward approach to treatment and while it might appear to be at odds with highly personalized medicine, it is a strategy that can reduce the global burden of cardiovascular disease, he added. One of the major problems in public health, said Fuster, is that people simply aren’t adhering to effective therapies, which is something the polypill strategy can improve.
One can begin to project the possibility that the results will be even more striking if the trial continues follow-up. Valentin Fuster
“This isn’t rocket science,” co-principal investigator José Castellano, MD, PhD (Centro Nacional de Investigaciones Cardiovasculares), told TCTMD. Castellano is lead author on the paper published simultaneously in the New England Journal of Medicine. “You’re just giving three class 1a-indicated drugs to people that need them and who will need them for the rest of their life. It’s really any patient after an MI who would benefit from this,” he explained.
Salim Yusuf MBBS (McMaster University/Population Health Research Institute, Hamilton, Canada), a longtime proponent of the polypill, said SECURE is yet more evidence showing the strategy is more effective than usual care to reduce cardiovascular events. Given the wealth of data, it’s time for physicians to seriously consider its use, he said.
“I’d like to see it utilized everywhere,” Yusuf told TCTMD. “Even in North America, in secondary prevention, the use of effective therapies is often under 40% or 50%.” Those numbers fall off even further as time goes on, he added.
By preventing readmissions for MI, stroke, and the need for revascularization, the polypill strategy can reduce the costs to the healthcare system. Yusuf, who led the TIPS-3 and HOPE-3 studies of the polypill in primary prevention, said they’ve performed modeling exercises suggesting the strategy is not only cost-effective, but possibly even cost-saving, in multiple settings, including North America.
“It’s a straw-man argument where people say this is only for poor countries,” said Yusuf.
Two Decades On
The polypill concept was first proposed roughly two decades ago when two physicians—Sir Nicholas Wald and Malcolm Law (both Wolfson Institute of Preventive Medicine, London, England)—argued that a single pill given to all adults 55 years and older could reduce the global burden of cardiovascular disease by 80%. Since then, that contentious strategy has been debated and refined somewhat, with research focusing instead on different patient populations who might benefit from a polypill.
Several trials in primary prevention—TIPS-3, PolyIran, and HOPE-3, as well as a meta-analysis that followed—all showed that the fixed-dose combination therapy could reduce the risk of major cardiovascular events.
This isn’t rocket science. You’re just giving three class 1a-indicated drugs to people that need them and who will need them for the rest of their life. José Castellano
In secondary prevention, proponents of the strategy believe it could reduce the risk of recurrent events by promoting greater adherence to treatments. In the FOCUS study, which was performed by Castellano, Fuster, and colleagues, the researchers showed that the polypill could significantly improve adherence over usual care in patients with a recent MI. Subsequent studies showed a strong association between patient outcomes and medication adherence.
With this background, the researchers launched the open-label SECURE trial, a study conducted at 113 hospitals in Spain, Italy, France, Germany, Poland, the Czech Republic, and Hungary and involving 2,499 patients (mean age 76 years; 31% women) with a recent type 1 MI. The median time between the index MI and randomization was 8 days. The mean systolic blood pressure was 129.1 mm Hg, and the mean LDL cholesterol level was 89.2 mg/dL at randomization.
The polypill contained aspirin 100 mg, the ACE inhibitor ramipril (2.5, 5, or 10 mg), and atorvastatin (20 or 40 mg). Physicians had the option of reducing the statin dose to 20 mg based on the patient’s history or blood-test results, but the majority received the higher dose (91.7%). The dose of the ACE inhibitor was started at 2.5 mg in ramipril-naive patients and gradually increased to 10 mg. The majority of patients (40.9%) received ramipril 2.5 mg, atorvastatin 40 mg, and aspirin 100 mg.
Patients randomized to usual care were treated according to the ESC guidelines, with 80% receiving high-intensity statin therapy, including atorvastatin 80 mg. Most of the patients in the usual-care group received ramipril, but other ACE inhibitors were part of treatment. Roughly 95% of patients in both the polypill and usual-care arm received an additional antiplatelet agent and more than 80% were also treated with beta-blockers.
Adherence at 6 months was significantly better in the polypill arm, with 70.6% of patients sticking to therapy compared with 62.7% of the usual-care patients. At 2 years, adherence remained significantly higher in the polypill study group (74.1% vs 63.2%). In terms of treatment effects, there was no significant difference in systolic and diastolic blood pressure between the two study arms at 2 years, nor was there any difference in mean LDL-cholesterol levels.
After a median follow-up of 3.0 years, the primary outcome occurred in 9.5% of patients treated with the polypill and 12.7% of patients treated with usual care (HR 0.76; 95% CI 0.60-0.96). The secondary endpoint—cardiovascular death, nonfatal MI, and nonfatal stroke—occurred in 8.2% of patients treated with the polypill and 11.7% of those who received usual care (HR 0.70; 95% CI 0.54-0.90). The benefit of the polypill was consistent across all subgroups, including those stratified by country, age, sex, and the presence/absence of diabetes, chronic kidney disease, or prior revascularization.
Investigators believe greater adherence to treatment explains the reduction in clinical outcomes. Given that there were no between-group differences in blood pressure and LDL cholesterol, Fuster hypothesized that the reduction in clinical events might be explained by the pleiotropic effects of statins, as well as ACE inhibitors.
“There’s good data following myocardial infarction that the statin can be anti-inflammatory and antithrombotic,” Fuster told TCTMD.
Yusuf also highlighted the lack of between-group difference in LDL cholesterol and blood pressure, a finding that suggests the benefit observed in SECURE—possibly half to two-thirds—could be attributable to aspirin.
In a discussion following the Hot Line presentation, Louise Bowman, MBBS, MD (University of Oxford, England), said that medication adherence remains a large problem in medicine. “Unless you swallow a tablet, it’s not going to work, no matter how small the P value was in the efficacy trial,” she said.
Despite the “extremely impressive” results, Bowman pointed out that SECURE does have some limitations, noting that it was completed during the COVID-19 pandemic. The trial missed its hoped-for enrollment of 3,200 patients and had a lower-than-expected event rate, leaving it somewhat underpowered. Also, the open-label design may have introduced some bias into the study, she said. Fuster agreed with Bowman’s assessment of limitations but said he doesn’t think they discredit the findings in any way.
“At the very end, I have to tell you with [all my] soul, this is a real study,” said Fuster. “In other words, I feel very strongly the data is telling us the polypill is a polypill of benefit.”
Adding to the Polypill
In Europe, this polypill, which was developed by Ferrer along with the Spanish Centro Nacional de Investigaciones Cardiovasculares, is commercially available in 25 countries. The US Food and Drug Administration also is planning to review the new SECURE data, said Castellano.
Citing results from the PURE study showing that the use of secondary prevention therapy is extremely poor, especially in low-income countries, Castellano said there is a need for a simple and effective treatment such as the polypill.
Nobody is saying the polypill should be the only treatment available. Salim Yusuf
“It would be a nice, global solution to imperfect accessibility,” he said, noting that treatments for HIV and hepatitis C frequently include multiple drugs in single tablet, treatments that have turned those killers into manageable chronic diseases. Castellano emphasized that the polypill needn’t be an “all-or-nothing strategy” and that physicians can still personalize treatment depending on the patient’s risk or test results, such as LDL cholesterol or blood pressure.
“You have a core treatment that is proven to be very beneficial, but you can tinker and personalize, especially now with all the weapons available for secondary prevention,” he told TCTMD. “You can still address residual risk on top of the polypill. The polypill ensures patients are going to be taking at least three active drugs and they’re going to be taking them enough to achieve optimal secondary prevention.”
Yusuf agrees.
“Nobody is saying the polypill should be the only treatment available,” he said. “The polypill should be one of the options and physicians can use the polypill with the knowledge that should they wish to add [other medications], they can do so. It’s not an either-or strategy. It doesn’t conflict with personalized medicine. It should just be used as a good foundation.”
In an editorial accompanying the published paper, Thomas Wang, MD (UT Southwestern Medical Center, Dallas, TX), says he believes the polypill deserves a role in clinical practice, but highlights the lack of commercial interest given that the medications are off patent. “Moving the polypill forward will likely require public and private partnerships, as exemplified by the SECURE trial,” he writes. “Doing so in the context of secondary prevention may be a good place to start.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Castellano JM, Pocock SJ, Bhatt DL, et al. Polypill strategy in secondary cardiovascular prevention. N Engl J Med. 2022;Epub ahead of print.
Wang TJ. The polypill at 20—what have we learned? N Engl J Med. 2022;Epub ahead of print.
Disclosures
- Fuster and Wang report no relevant conflicts of interest.
- Yusuf reports grants from the Canadian Institutes of Health Research, Wellcome Trust, AstraZeneca, and Cadila Pharmaceuticals related to HOPE-3 or TIPS-3. He previously reported honoraria/travel expenses from AstraZeneca, Bater, Boehringer Ingelheim, and Ferrer.




Comments