One Pill to Treat Them All: Polycap Strategy Sees Success in TIPS-3
Use of a polypill plus aspirin may be a way to reduce the global burden of ASCVD, even in some parts of US.
When used alongside aspirin, a fixed-dose combination tablet that includes a statin, ACE inhibitor, beta-blocker, and diuretic significantly lowered the risk of adverse cardiovascular events in a large primary-prevention population at intermediate risk for atherosclerotic cardiovascular disease (ASCVD), according to data presented today at the virtual American Heart Association 2020 Scientific Sessions.
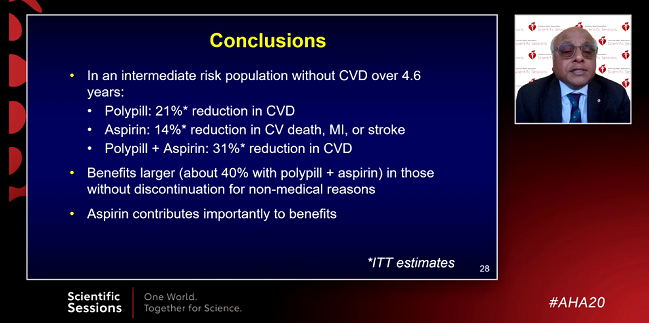
However, for patients treated with polypill alone, which includes simvastatin 40 mg, atenolol 100 mg, ramipril 10 mg, and hydrochlorothiazide 25 mg, there was a borderline statistically significant reduction in the risk of the primary composite endpoint when compared with placebo-treated patients. After a mean follow-up of 4.6 years, the primary endpoint had occurred in 4.4% of patients treated with the polypill versus 5.5% among those treated with placebo (HR 0.79; 95% CI 0.63-1.00).
Salim Yusuf, MD (McMaster University/Population Health Research Institute, Hamilton, Canada), who led the international study along with Prem Pais, MD (St. John’s Research Institute, Bangalore, India), said the observed reduction in ASCVD events with the polypill and aspirin was less than originally hypothesized. But he stressed it is still important, not only for low-income countries but also globally. The top-enrolling countries were India, the Philippines, Columbia, and Bangladesh; Canada enrolled 131 patients.
“I think it’s absolutely incorrect to say that this is only applicable to poor countries,” said Yusuf during a morning press conference. “Why wouldn’t rich countries also benefit from [the polypill]? Further, we estimate that if half of people eligible to use the polypill—that is, half of the hypertensives and half of the diabetics—we would prevent 3 to 5 million cardiovascular disease events per year, with a quarter of them from rich countries. If the rich countries don’t want that benefit, that’s their prerogative.”
I think it’s absolutely incorrect to say that this is only applicable to poor countries. Salim Yusuf
Yusuf said a polypill fixed-dose combination tablet is likely a cost-effective strategy, or at least cost neutral, although it will depend on the drug’s price. In India, it costs roughly 33 cents per day, making it cost neutral. He imagines more potent polypill combinations to emerge, with these agents capable of reducing LDL cholesterol and blood pressure to a greater extent, “which may lead to larger benefits.”
Not everybody is convinced that polypill approach would work in the United States, or in other high-income countries for that matter. Steven Nissen, MD (Cleveland Clinic, OH), called the polypill a “terrible idea.” For starters, he expressed consternation with use of simvastatin 40 mg given the large number of potential drug interactions with the agent, as well as with atenolol 100 mg. The high dose reduces exercise tolerance and can cause significant side effects, among them erectile dysfunction.
“Why throw the kitchen sink at people without thinking about it?” Nissen told TCTMD. “Modern medicine is about customizing therapy for individuals. What if somebody has an LDL cholesterol of 50 mg/dL? Do you really want to give them simvastatin with its risks? My blood pressure happens to run 100/60 [mm Hg]. What do you think would happen if I took three antihypertensive drugs? So really there are huge, huge issues here. This might be an effective strategy for third-world countries, but even there I’m not sure. . . . I don’t think this is a good strategy.”
Factorial Design
In TIPS-3, investigators randomized 5,173 participants to determine if a fixed-dose combination tablet reduced the risk of major cardiovascular outcomes in a primary prevention population. As part of the factorial design, the additional interventions included aspirin alone compared with placebo as well as polypill plus aspirin compared with double placebo. Men 50 years and older and women 55 years and older with an INTERHEART risk score ≥ 10 (or men and women 65 years and older with an INTERHEART risk score ≥ 5) were included in the international study. Roughly 53% of study participants were women. Mean LDL cholesterol level and systolic blood pressure at baseline were 121 mg/dL and 144.5 mm Hg, respectively.
Why throw the kitchen sink at people without thinking about it. Steven Nissen
Treatment with the polypill resulted in nearly a 10-mm Hg decrease in systolic blood pressure, but the reduction attenuated over time such that the final mean difference between the treatment and placebo groups was 5.8 mm Hg. With respect to LDL cholesterol, the mean difference was 19.0 mg/dL between the polypill- and placebo-treated patients.
Nonadherence was 19% at 2 years, 32% at 4 years, and 43% at the completion of the trial, and these rates were similar for those taking the polypill and placebo. Speaking with the media, Yusuf said there were administrative and logistical challenges supplying the polypill to patients, and that this problem was further exacerbated by the COVID-19 pandemic.
For the polypill versus placebo, the reduction in cardiovascular death, MI, stroke, heart failure, resuscitated cardiac arrest, and revascularization bordered on significance (P = 0.05). When investigators performed a prespecified sensitivity analysis that accounted for nonadherence, there was a statistically significant 26% reduction in the primary outcome with the polypill in patients who stopped taking the drugs for less than 30 days for nonmedical reasons (HR 0.74; 0.57-0.97). Dizziness or hypotension rates were more frequent in the polypill arm (2.7% vs 1.1% with placebo), as was cough, but there was no signal of muscle pain or weakness.
For the polypill plus aspirin versus double placebo, there was significant benefit with treatment, with the combination reducing not only the primary endpoint but also other secondary endpoints, including cardiovascular death, MI, or stroke. In the sensitivity analysis that focused on patients who stopped the medication for less than 30 days, the observed reduction in the primary endpoint with the polypill plus aspirin combination was nearly 40% (HR 0.61; 95% CI 0.41-0.91). Aspirin alone did not reduce the risk of major cardiovascular events compared with placebo, but there was a trend toward benefit. Additionally, there was a statistically significant reduction in the risk of stroke among those treated with aspirin compared with those who received placebo.
Polypill Plus Aspirin vs Double Placebo: 4.6-Year Follow-up
|
|
Polypill + Aspirin (n = 1,429) |
Double Placebo (n = 1,421) |
HR (95% CI) |
|
Primary Endpoint* |
4.1% |
5.8% |
0.69 (0.50-0.97) |
|
Cardiovascular Death, MI, Stroke |
3.6% |
5.3% |
0.68 (0.47-0.96) |
|
Primary Endpoint + Angina |
4.3% |
6.1% |
0.69 (0.50-0.96) |
*Cardiovascular death, MI, stroke, heart failure, cardiac arrest, and revascularization
Aspirin vs Placebo: 4.6-Year Follow-up
|
|
Polypill + Aspirin (n = 2,860) |
Double Placebo (n = 2,853) |
HR (95% CI) |
|
Primary Endpoint* |
4.1% |
4.7% |
0.86 (0.67-1.10) |
|
Cardiovascular Death |
3.0% |
3.5% |
0.85 (0.64-1.14) |
|
MI |
0.8% |
0.7% |
1.04 (0.57-1.89) |
|
Stroke |
0.8% |
1.4% |
0.58 (0.35-0.98) |
* Cardiovascular death, MI, or stroke
With respect to aspirin in primary prevention, the American College of Cardiology and American Heart Association (ACC/AHA) guidelines downgraded their recommendation recently, now stating that aspirin use in older individuals (> 70 years) and those with an increased risk of bleeding is not recommended (class III recommendation). For middle-aged adults, those 40 to 70 years old, aspirin might be considered for primary prevention if they are at higher risk for CVD but do not have an excessive risk of bleeding (class IIb recommendation).
Those recommendations were based on the results of three recent trials: ASPREE, ARRIVE, and ASCEND. However, Yusuf noted the benefit of treatment observed in TIPS-3 includes the use of aspirin and their nonsignificant 14% reduction in major CVD events with aspirin alone versus placebo lines up with a recent meta-analysis.
Donald Lloyd-Jones, MD (Northwestern University Feinberg School of Medicine, Chicago, IL), who moderated the media briefing, said that aspirin did significantly reduce the risk of major vascular events in ASCEND, but it was the risk of major bleeding in that and other trials that tipped the scale against its widespread use.
This could be a game changer in terms of preventing large numbers of cardiovascular events. Donald Lloyd-Jones
“Context is really important,” he said. “I think we saw smaller benefits in some of those [aspirin primary prevention] trials, sometimes not significant in terms of cardiovascular disease reduction. Many of those trials were done in settings where there had been longstanding engagement of preventive therapies with the health system in higher-resource settings. Aspirin didn’t have as much room, I would say, to provide benefit. In settings where patients might not have been as engaged as equally with the health system or preventive strategies, and perhaps have worse risk factors, there is more room aspirin to add benefit, particularly when used as an additional strategy rather than when used later once blood pressure and cholesterol are already controlled.”
Yusuf agreed, noting that they used just 75 mg of aspirin. “The key is to reduce the dose and get the benefits without the harm,” he told TCTMD. “I would say that aspirin chosen carefully does have a role in primary prevention, along with lifestyle [changes] as well as the other polypill components.”
Global Implications
Anushka Patel, MBBS, PhD (The George Institute for Global Health, Sydney, Australia), who commented on the study during the morning press conference, said that while TIPS-3 was conducted largely in middle-income countries, the results should have a global impact. Patel pointed out the previous studies have shown the polypill strategy can lead to significant reductions in blood pressure and LDL cholesterol among disadvantaged US populations.
“Based on the collective evidence we now have, also with TIPS-3 on clinical endpoints, it’s hard to argue against the potential value of a polypill approach in such a population, and I think, therefore, it really does the emphasize the global relevance of this trial and other polypill trials,” said Patel.
Lloyd-Jones called TIPS-3, and the polypill strategy in general, paradigm-shifting. “This is applicable to settings worldwide,” he said. “We have seen this work in high-income countries. I think it’s particularly attractive when we apply it to low-resource settings, though.” With the hope that adherence would be better outside a clinical trial hampered by COVID-19, and with the strategy likely cost-effective or cost neutral, the polypill strategy can help overcome some of the treatment barriers endemic to settings with limited resources, said Lloyd-Jones.
“This could be a game changer in terms of preventing large numbers of cardiovascular events,” he said.
R. Todd Hurst, MD (Banner—University Medicine Heart Institute, Phoenix, AZ), who wasn’t involved in the study, isn’t certain the polypill is a strategy that would catch on in the United States. Many patients would be reluctant to take a drug where “one size fits all,” although there may be populations where that blanket approach might be a good fit, he said. “The concept of the polypill is well intentioned—how can we get more lifesaving medications to more people?—but I think executing that has its challenges. In my experience, outside of a research setting I don’t know where it’s been done on a widescale basis with success.”
Hurst, who has a diverse clinical practice including patients in an underserved community, said there is reluctance to take medications “unless there’s a really compelling reason” to do so. “Unless it’s an active problem that somebody has, it can be challenging to get them to adhere to recommendations,” he said. The polypill strategy, which is intended to reduce the risk of ASCVD in primary prevention, would be a tough sell for patients, he thinks. As for the aspirin finding, Hurst said if there is any role its use, and “there probably isn’t,” it’s only going to be highly select populations. TIPS-3, he said, doesn’t change his mind on aspirin for primary prevention.
No Safety Concerns
During the discussion, Patel said there are now data from three studies—TIPS-3, PolyIran, and HOPE-3—supporting the polypill concept, with these showing an average 20% to 30% reduction in major cardiovascular events.
“None of these trials, including TIPS-3, have identified any safety concerns,” she noted. However, Patel said that the reduction in blood pressure and cholesterol in TIPS-3 was approximately 40% lower than what would be anticipated based on the drugs included in the fixed-dose combination tablet. The lower than expected treatment differences are not explained by increased use of medical therapy in the placebo arm, nor are they fully explained by lack of adherence. As for whether or not aspirin should be included as part of the polypill for primary prevention in intermediate-risk patients can’t be answered from this study, and the decision to use aspirin should be individualized, she said.
Nissen ultimately remains skeptical about the approach, including adding aspirin for primary prevention, even at a low dose, in large swath of patients. Moreover, he said the drugs and dosages used in the TIPS-3 polypill are a “particularly noxious combination.”
To TCTMD, Hurst said the high dosages also caught his attention, noting: “The typical polypill strategy has been modest or intermediate dosages of medications, where this is using a high dose of simvastatin and a high dose of atenolol. Also, the choices. Simvastatin just isn’t used very much anymore because we have other choices that have less chance of drug-drug interaction. The biggest surprise for me is atenolol 100 mg, though. That’s not a first-line agent in treating blood pressure. It’s not a medication that has any indication in a primary prevention patient. So, it’s a surprising choice, although I know there is always a debate about the drugs used in these polypills.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Yusuf S, Joseph P, Dans A, et al. Polypill with or without aspirin in persons without cardiovascular disease. N Engl J Med 2020;Epub ahead of print.
Disclosures
- Pais reports institutional fees/reimbursement from Cadila Pharma for serving as the national coordinating center for India.
- Yusuf reports grants from the Wellcome Trust.


Comments