POPCORN: Hemodialysis Patients Fare Well With Tailored PAD Therapies
The frequent exclusion of such patients from trials makes real-world data like these valuable for clinicians, says Eric Secemsky.

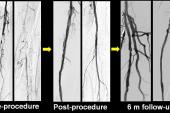
Patients with peripheral artery disease (PAD) who are on hemodialysis have worse patency outcomes after endovascular interventions with drug-coated balloons (DCB) than patients not on dialysis, but their limb salvage rates at 3 years are still well over 90%, according to data from the real-world, multicenter POPCORN registry in Japan.
At 3 years, the estimated rate of freedom from restenosis was 62.8% in the hemodialysis group and 67.3% in those not on dialysis. No below-the-knee runoff, prior endovascular procedures, popliteal lesions, and severe calcification and dissection each were independent predictors of poorer primary patency for dialysis-treated patients.
“These findings support the need for tailored endovascular strategies in [hemodialysis] patients, integrating lesion complexity, device selection, and vascular biology,” write Yasutaka Yamauchi, MD, PhD (Takatsu General Hospital, Kawasaki, Japan), and colleagues in a paper published July 14, 2025, in JACC: Cardiovascular Interventions.
They note that patients on dialysis are a high-risk group for complications after endovascular therapies for PAD, including having a greater risk of death and major limb amputation. Because of these risks, as well as a greater chance of endovascular therapy not being unsuccessful, this patient subset is often not included in studies and objective performance goals of endovascular therapies, leaving gaps in understanding about how well they do after interventions.
To TCTMD, Eric Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), said that is challenging for clinicians who routinely manage hemodialysis patients with PAD.
“Many of our patients have renal insufficiency and a portion of those have end-stage renal disease and are on hemodialysis, but you are applying data from a completely different group to this very specific group on dialysis, never knowing whether these devices really function as well,” he said.
Secemsky, who co-wrote an accompanying editorial with Maxime Dubosq-Lebaz, MD (Beth Israel Deaconess Medical Center), said that while the POPCORN data aren’t really surprising, they confirm some known predictors of poor outcomes and provide reassurance that by working around the patient’s dialysis schedule and needs, it is possible to get durable results in many of them.
“A big question that comes up with this patient group is if they’re dialysis dependent and they have peripheral artery disease that's symptomatic or even severe, as in the case of CLTI [chronic limb-threatening ischemia], are they still a candidate for [kidney] transplant? That's when you really have to work in a multidisciplinary group, in particular with transplant, about whether they can still get transplanted and be on the anti-rejection medications,” he said. “Much of what goes into managing these patients requires a lot of collaboration and discussion, not necessarily only around their dialysis, but just general prognosis and what the overall plan is for that patient.”
POPCORN Provides Food for Thought
The POPCORN analysis included 2,507 patients with Rutherford category 2-5 PAD who underwent DCB treatment at 81 cardiovascular centers in Japan. Of these, 728 patients (mean age 72 years; 34% women) were on hemodialysis and 1,779 patients (mean age 76 years; 35.5% women) were not.
In addition to being younger, the dialysis group also had a higher incidence of diabetes and heart failure, and they were more likely to be nonambulatory and CLTI. Popliteal lesions were more common in the dialysis group, while chronic total occlusions were less common. The IN.PACT Admiral DCB (Medtronic) was used in 70% or more of patients in both groups, with the remainder being the first-generation Lutonix DCB (Bard).
Follow-up included routine monitoring with ankle-brachial index and vascular duplex ultrasound after 1 and 12 months and then every 12 months annually for up to 5 years, regardless of the presence of ischemic symptoms.
Freedom from target lesion revascularization was 69.7% in the hemodialysis group at 3 years versus 80.3% in the nondialysis group. Additionally, limb salvage rates were 93.6% and 98.9%, respectively, at 3 years, with overall survival rates of 60.0% and 84.7%.
The findings were similar after propensity-matched scoring.
In an adjusted analysis of baseline characteristics and their association with restenosis at 3 years, severe dissection (grade D or higher) was associated with the greatest risk (RR 1.99; 95% CI 1.11-3.57), followed by history of endovascular therapy (RR 1.88; 95% CI 1.37-2.57), no below-the-knee runoff (RR 1.60; 95% CI 1.16-2.19), bailout stenting (RR 1.49; 95% CI 0.76-2.92), no slow flow after DCB (RR 1.41; 95% CI 0.72-2.77), severe calcification (RR 1.39; 95% CI 1.07-1.81), popliteal lesion (RR 1.36; 95% CI 1.06-1.75), anticoagulant use (RR 1.34; 95% CI 0.92-1.95), and use of Lutonix versus In.PACT Admiral DCB (RR 1.32; 95 CI 1.02-1.70).
Yamouchi and colleagues say the findings suggest that balloon dilation, uniform drug penetration, and use of a DCB with high drug dose like IN.PACT Admiral rather than the low-dose Lutonix are all associated with better outcomes in hemodialysis patients. Additionally, while debulking devices were not used in the preparation phase of POPCORN, the researchers suggest that they should be considered in the subset of patients with severely calcified lesions to allow for better drug delivery.
Much of what goes into managing these patients requires a lot of collaboration and discussion, not necessarily only around their dialysis, but . . . what the overall plan is. Eric Secemsky
In their editorial, Secemsky and Dubosq-Lebaz note that POPCORN, which showed the importance of calcium scoring in this population, as well as a post-hoc analysis of the BEST-CLI trial that showed dialysis status to be a dominant modifier of death and limb outcomes, help point the way toward closing gaps in the care of PAD in dialysis-dependent patients.
They also highlight emerging options for achieving better patency that are under investigation, including sirolimus-coated balloon platforms as an alternative to standard paclitaxel. However, the exclusion of hemodialysis patients from several of these studies will once again limit their interpretation, they add.
Other potential new options that remain to be explored for improving vascular healing and lowering the risk of restenosis in this population are agents that modulate inflammation, oxidative stress, or vascular calcification.
To TCTMD, Secemsky said one of the most important things that the POPCORN findings underscore is that not all hemodialysis patients with PAD are the same, showing the need to better characterize and incorporate predictive variables from real-world populations into practical risk models.
“We really need to be including some of these variables like ambulatory status, which is an important proxy for frailty,” he said. “A younger, functional patient who has some congenital reason they are on dialysis is very different [from] an older, nonambulatory patient with multiple comorbidities. So, we need to better understand which hemodialysis population we’re dealing with when considering outcomes.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Yamauchi Y, Takahara M, MD, Soga Y, et al. Vessel patency after femoropopliteal drug-coated balloon therapy in patients on hemodialysis. JACC Cardiovasc Interv. 2025;18:1660-1670.
Dubosq-Lebaz M, Secemsky EA. Reviving hope: the impact of drug-coated balloons in high-risk PAD patients on hemodialysis. JACC Cardiovasc Interv. 2025;18:1671-1674.
Disclosures
- The POPCORN study was supported by the Research Association for Lower Limb Artery Revascularization.
- Yamauchi and Dubosq-Lebaz report no relevant conflicts of interest.
- Secemsky reports institutional grants from Abbott/CSI, BD, Boston Scientific, Cook, Medtronic, and Philips; and speaking/consulting fees from Abbott/CSI, BD, BMS, Boston Scientific, Cagent, Conavi, Cook, Cordis, Endovascular Engineering, Gore, InfraRedx, Medtronic, Philips, RapidAI, Rampart, Shockwave, Siemens, Teleflex, Terumo, Thrombolex, VentureMed, and Zoll.



Comments