Post-TAVI Pacemaker Rates Down in the US, but ‘Still Quite High’
As TAVI is performed in younger, low-risk patients, rates of 10% to 15% aren’t going to be acceptable, Bernard Prendergast says.

MIAMI, FL—Rates of permanent pacemaker implantation within 30 days of TAVI have come down over time in the United States, although there remains a need for further improvements, data from the Society of Thoracic Surgeons/American College of Cardiology TVT Registry show.
Between October 2013 and February 2020, the trend was significant for both balloon-expandable and self-expanding valves (P < 0.001 for both trends), although the decline was more pronounced for the latter, Katherine Chau, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), reported here at TVT 2021 yesterday.
The switch to new-generation versus first-generation devices was associated with lower odds of pacemaker implantation only for self-expanding valves (OR 0.71; 95% CI 0.65-0.78). Annual procedure volume at the hospital level didn’t appear to influence the need for a pacemaker, although rates came down as case numbers for individual operators increased, “suggesting the potential impact of a learning curve,” Chau said.
Despite the overall positive trends, “the rates are still quite high,” Bernard Prendergast, MD (St Thomas' Hospital, London, England), commented after Chau’s presentation, which showed rates in the last year of the study period of 9.29% for balloon-expandable valves and 15.6% for self-expanding valves.
“As we’re moving into younger, low-risk patients, rates of 10% or 15%, whichever valve you’re using, are not going to be acceptable,” Prendergast said. “So we need to keep improving, we need to implant those valves high, and we need to take all precautions that we can to reduce this complication in our younger patients.”
A Frequent and Important Complication
Permanent pacemaker implantation remains a frequent and important complication of TAVI, both clinically and economically, Chau said. Multiple factors may have contributed to lowering rates over the years—including technological advances and accumulating experience at the operator and hospital levels—but prior studies examining this possibility have provided mixed results, she said.
To further explore the issue, Chau et al examined data from the TVT Registry. After excluding patients who already had permanent pacemaker or an implantable cardioverter-defibrillator, they were left with 144,042 patients treated with a balloon-expandable valve and 52,965 treated with a self-expanding valve.
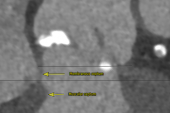
First-generation valves included the Sapien and Sapien XT (Edwards Lifesciences) on the balloon-expandable side and the CoreValve (Medtronic) on the self-expanding side. New-generation devices included Sapien 3 and Sapien 3 Ultra and the CoreValve Evolut R and Evolut PRO. These valves took over for the older ones around 2015, coinciding with regulatory approval.
Generally, patients treated with the new-generation valves tended to be younger and to have fewer comorbidities and lower STS scores, which is not surprising considering the changing indication for TAVI over time, Chau said. Procedures with the newer devices also were less likely to involve general anesthesia and more likely to be performed with femoral access.
In contrast to what was seen with self-expanding valves, the likelihood of permanent pacemaker implantation was no different when comparing new- and old-generation balloon-expandable valves (OR 1.03; 95% CI 0.97-1.10).
The lack of an association between annual TAVI volumes at the center level (P = 0.258) and the relationship between higher operator case numbers and lower pacemaker rates (P < 0.001) were consistent for both types of prostheses.
Chau noted that “due to the observational nature of this analysis and baseline differences in populations treated with different valve types, no statistical comparisons were attempted between the two groups.”
Discussing Pacemaker Risks With Patients
Tamim Nazif, MD (NewYork-Presbyterian/Columbia University Irving Medical Center), commenting in a panel discussion after Chau’s presentation, said it’s challenging to identify what is driving the reductions in pacemaker rates over time. Although it could be related to technological improvement, it’s difficult to separate that issue from other factors that were not included in the TVT Registry, he said. That includes information on certain procedural techniques, including depth of implantation, which he pointed out is of particular importance when talking about pacemaker rates.
Another thing to consider, according to Gorav Ailawadi, MD (University of Michigan, Ann Arbor), is that patients treated with TAVI have been getting healthier over time, which could be contributing to the trends in pacemaker rates.
Everyone agreed, however, that regardless of the reasons underlying the declining need for pacemakers after TAVI, there is still an opportunity to make headway. “It’s a great and well-taken point,” Nazif said, alluding to Prendergast’s comments, “that while things are improving, they’re improving slowly and they need to get better.”
That point is underscored by some data showing that pacemaker implantation is associated with worse clinical outcomes. Nazif noted that a meta-analysis published last year demonstrated that permanent pacemaker implantation after TAVI correlated with increased risks of all-cause mortality and heart failure rehospitalization (but not cardiac death) at 1 year.
“Now as we move into younger and lower-risk patients, we really need to think about the not just 1-year outcomes, but what are the 5-, 10-, 20-year implications of getting a pacemaker,” Nazif said, adding that pacemaker risks are discussed with patients.
Ailawadi agreed that it has to be part of the considerations when thinking about lifetime management of patients, particularly as TAVI moves into younger people and those with bicuspid valves. “Not just what are we going to do when this valve fails, whether it’s a SAVR, TAVR, whatever, and will we have room for another valve in TAVR, for example,” he said. “We should probably also have that discussion with them: ‘Hey, this is your risk of a pacemaker [and] this is what that means in terms of your long-term mortality.’”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Chau K. Trends in permanent pacemaker implantation after TAVR: an STS/ACC TVT Registry analysis. Presented at: TVT 2021. July 22, 2021. Miami, FL.
Disclosures
- The study was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry and the Society of Thoracic Surgeons National Database.
- Chau reports no relevant conflicts of interest.




Comments