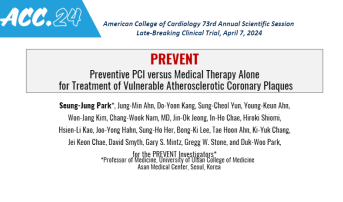
PREVENT Supports Early PCI for Vulnerable Plaque, With Reductions in MACE
The study may raise more questions than it answers, particularly around the idea of what constitutes “vulnerable.”
ATLANTA, GA—Compared with optimal medical therapy (OMT) alone, a preventative strategy of PCI to treat vulnerable plaques on top of OMT may reduce the incidence of serious CV events over the next 2 years, the PREVENT trial investigators conclude.
In the trial, patients randomized to the prophylactic group had an 89% lower risk of the composite primary endpoint of cardiac death, target-vessel MI, ischemia-driven target vessel revascularization, or hospitalization for unstable or progressive angina at 2 years compared with those in the OMT group.
The trial was met with mixed reactions, however.
Mamas A. Mamas, BMBCh, DPhil (Keele University, Stoke-on-Trent, England), said the study provides a strong signal of support for its value in heading off future events.
“It's still too early to be advocating treating every vulnerable plaque that you see, but it’s an interesting piece of data because we all commonly see high-risk features that we know predict future events, but we don’t know what we should do about them,” he said.
Interestingly, most of the benefits of the prophylactic PCI to stabilize high-risk plaques and reduce risk of rupture occurred within the first 2 years.
“There are a number of reasons why this may have occurred. The development of these high-risk phenotypes, these vulnerable plaques, is not a static phenomenon. You may treat one of the vulnerable plaques that you've seen on OCT, but 2 or 3 years down the line, you're going to get new ones that are developing that you're not going to be treating. I guess that's where we really need to sort of take a more holistic approach in these patients,” Mamas added. “It's not just stenting lesions that we think are high risk, but thinking how do we prevent events in future high-risk lesions. That's where you need the really aggressive secondary prevention and utilization of therapies that have been shown to impact on plaque morphology.”
These would include agents like PCSK9 inhibitors, he added, which have been shown in studies like YELLOW III to improve plaque morphology in stable CAD. Problematic in PREVENT, however, is that less than 2% of patients in the trial were on a PCSK9 inhibitor, PREVENT senior investigator Duk-Woo Park, MD, PhD (Asan Medical Center/University of Ulsan College of Medicine), told TCTMD.
In a press conference following the presentation, Marc P. Bonaca, MD (University of Colorado School of Medicine, Aurora), noted that the PREVENT data are thought-provoking and potentially a paradigm shift for the future, but to TCTMD he said the strategy is not “ready for prime time.”
Instead, Bonaca said the next step would be to look at questions that remain and could potentially be answered in future studies.
“Maybe in sham-controlled studies like ORBITA, maybe [by exploring] harder endpoints, because revascularization is something in an unblinded trial that you have to be a little careful about,” he added.
Sustained Reduction in Events to 7 Years
PREVENT enrolled 1,606 patients (mean age 64 years; 27% women) at 15 centers in four countries who had non-flow-limiting vulnerable coronary plaques of > 50% stenosis and negative fractional flow reserve (FFR) of > 0.80. Vulnerable plaques were defined as lesions possessing at least two of these characteristics: minimal lumen area ≤ 4.0 mm2 by intravascular ultrasound or optical coherence tomography, plaque burden > 70% by intravascular imaging, thin-cap fibroatheroma (TCFA) detect by OCT or radiofrequency IVUS, and lipid-rich plaque detected by NIRS. Ultimately, 95% of patients in the trial were assessed by grayscale intravascular imaging, not newer, more sensitive imaging modalities.
Patients were randomly assigned to PCI plus OMT or OMT alone. The trial was initially designed to use bioresorbable scaffolds, but after these were removed from the market, permanent metal stents were used. As a result, in the PCI group, DES were used in 67% and bioresorbable scaffold in 33%. Intravascular imaging was used in all cases to optimize stent or scaffold implantation.
More than 50% of patients in both groups were on high- or moderate-intensity statins plus ezetimibe during the follow-up period. The mean LDL-cholesterol level in both groups was 64 mg/dL at last follow-up, down from a median of 83 mg/dL at baseline in the preventive PCI group and 93 mg/dL in the OMT group.
At 2 years, the rate of the primary outcome was 0.4% in the preventive PCI group and 3.4% in the OMT group (HR 0.11; 95% CI 0.03-0.36). Over long-term follow-up, the primary outcome occurred less frequently in the preventive PCI group than in the medical therapy alone group (6.5% vs 9.4%; HR 0.54; 95% CI 0.33-0.87). The 3% absolute difference in the primary composite endpoint was sustained through 7 years of follow-up (median 4.4 years).
The number-needed-to-treat (NNT) to prevent one primary outcome event over 2 years was in the preventive PCI group was 45.4, with a NNT of 87.7 to prevent one cardiac death or target-vessel MI.
In an analysis of the patient-oriented composite outcome (death from any cause, any MI, or any repeat revascularization, the preventive PCI group had consistently lower incidence rates at 2 years and 7 years (log-rank P = 0.022).
A question asked both by Bonaca and session panelist J. Dawn Abbott, MD (Brown University, Providence, RI), centered on the problem of determining what constitutes a “vulnerable” plaque?
ORBITA lead author Rasha Al-Lamee, MBBS, PhD (Imperial College London, England), pointed out to TCTMD that modern-day vulnerable-plaque trials have used OCT or NIRS. “For me, the PREVENT trial didn’t show patients with vulnerable plaque per se, but patients with high plaque burden,” Al-Lamee explained. “We’ve known for a long time that if they are physiologically negative, if lesions are non-flow-limiting, the right thing to do is to give them very intense lipid-lowering therapy, manage their risk factors.”
She continued: “I do think that there’s a future in terms of thinking about vulnerability and how it predicts events and what we might do about it.”
Al-Lamee also noted that the proportion of patients who had highly sensitive imaging like OCT and NIRS to look for vulnerable plaque was very low. “Our ability to detect from grayscale IVUS is not in the same league,” she concluded.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Park S-J, Ahn J-M, Kang D-Y, et al. Preventative PCI versus optimal medical therapy alone for the treatment of vulnerable atherosclerotic coronary plaques (PREVENT): a multicentre, open-label, randomized controlled trial. Lancet. 2024;Epub ahead of print.
Disclosures
- The study was funded by the Cardiovascular Research Foundation, Abbott, Yuhan, CAH-Cordis, Philips, and Infraredx.
- Park reports research grants and speaker fees from Abbott Vascular, Medtronic, Daiichi-Sankyo, ChongKunDang, Daewoong, and Edwards.




Comments