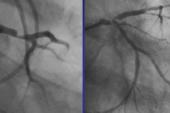
Provisional Stenting Noninferior to Planned Two-Stent Strategy for Left Main Disease: EBC MAIN
The lead investigator advised not “prejudging” the situation by deciding on a two-stent strategy from the outset.

A provisional approach to stenting left main bifurcation lesions is noninferior to an upfront two-stent strategy, according to results of the EBC MAIN study.
At 1 year, the primary composite endpoint of death, MI, and TLR was 14.7% in the provisional-stenting group and 17.7% in the upfront dual-stenting group (HR 0.8; 95% CI 0.5-1.3), said lead author David Hildick-Smith, MD (Brighton and Sussex University Hospitals, Brighton, England), in his presentation this week at EuroPCR 2021. The results were simultaneously published in the European Heart Journal.
According to Hildick-Smith, the most important takeaway of the study “is that it's not necessary to prejudge the issue and start with a nonprovisional technique, which therefore you can't modify; you’re committing straightaway to two steps. It’s not necessary to do that. Patients are equally well treated with a stepwise, layered provisional approach starting with a single stent as they are with a more complex dual-stent implant.”
While some prior studies like BBC ONE and NORDIC have suggested that mortality might be worse with a dual-stent approach in true left main bifurcations, the randomized DKCRUSH-V showed the opposite and formed the basis for a 2018 European Society of Cardiology recommendation that supports double-kissing crush over a planned provisional strategy.
You start with provisional, and then you go step-by-step until you achieve acceptable results, and then you stop. Goran Stankovic
In a discussion following the presentation, co-author Jens Flensted Lassen, MD, PhD (Odense University Hospital, Denmark), said he felt that the neutral results of EBC MAIN support the provisional approach because “it's very easy to keep it simple and reduce the number of stents, and reduce the complexity of the procedure, reduce dyes, X-rays, et cetera, and reduce the risk for the patient.”
One notable feature of the study is that intravascular imaging was not mandated.
“I was really keen to have imaging randomized within this study, and I’m now sorry that we didn’t manage to do that,” Hildick-Smith said in the discussion. Citing pushback from some operators about when to use it, as well as issues with reimbursement, he added, “a third of the patients had intravascular imaging. You might think it would have been more. It’s not dissimilar, actually, to what was seen in DKCRUSH, as well.”
Speaking with TCTMD, Mamas Mamas, BMBCh, DPhil (Keele University/Royal Stoke University Hospital), who was not involved in EBC MAIN, said he was surprised that intravascular imaging wasn’t mandated given that in left main cases, it helps operators to fully understand the anatomy, plan the procedure, and achieve optimal stent deployment. Mamas cited a 2014 study he was involved in, one that included over 11,000 left main procedures performed in England and Wales, showing that 50% of those involved intravascular imaging. Moreover, the study also found a 30% decrease in mortality at 1 year with the use of intravascular imaging.
“It's 7 years down the line, and yet in a randomized controlled trial undertaken in expert centers with lower-risk patients, intravascular imaging use is less than we see if the real world. That certainly raises eyebrows,” he said. Mamas pointed out that EBC MAIN also had high use of calcium modification techniques, which he said makes it even more surprising that imaging wasn’t required in order to help guide optimal calcium treatment strategy and to optimize the results.
“I suspect that had imaging been mandated, there would have been much lower rates of adverse events. Apart from cost, I don’t see the downside. Imaging can actually make your cases more straightforward because you know the degree of calcium in there, so you can use the appropriate treatments at the appropriate time rather than guessing and then having to go through a cascade of treatments until you get the right one,” Mamas said. “I think it's clear that you should not be undertaking left main PCI without using intravascular imaging. At the end of the day, we know that surgery has good outcomes for patients with left main disease, and we owe it to our patients to have outcomes either as close to, or as good as, surgery as possible.”
Advocating for Step-by-step
EBC MAIN was designed to examine clinical outcomes in 467 patients from 11 European countries who were randomized to either a stepwise, layered provisional strategy (n = 230) or systematic dual-stent approach (n = 237). The stent technique (culotte, DK-minicrush, T/TAP) was left to the discretion of the operator, but proximal optimization and kissing balloon technique were mandated in both groups.
In addition to seeing no differences in the primary endpoint by stent strategy at 1 year, the investigators reported no significant disparities in any of the individual components of the primary endpoint. Rates of definite/probable stent thrombosis also were similar at 1.7% in the provisional arm and 1.3% in the upfront double stenting group (P = 0.9).
The dual-stent group had longer procedure durations, fluoroscopy times, and higher X-ray doses, as well as a higher technical success rate, although procedural success was higher in the provisional group.
Of patients randomized to the dual-stent strategy, 5% needed only a single stent, while 22% of those randomized to provisional stenting required a second stent. In a press conference prior to his presentation, co-author Goran Stankovic, MD, PhD (University of Belgrade, Serbia), told TCTMD that it was not possible to differentiate those who eventually needed the second stent.
“There was [not] any single predictor for the occurrence of second stent implantation in the provisional [group], which could be also the result of a relatively low total number of patients included,” he said. In terms of the clinical message, he agreed with Hildick-Smith, stating that “you start with provisional, and then you go step-by-step until you achieve acceptable results, and then you stop.”
You should not be undertaking left main PCI without using intravascular imaging. . . . We know that surgery has good outcomes for patients with left main disease, and we owe it to our patients to have outcomes either as close to, or as good as, surgery as possible. Mamas Mamas
Hildick-Smith said he considered the EBC MAIN results to be “broadly good” for the treatment of left main disease. “There were fewer serious adverse events with the stepwise provisional approach, numerically, if not statistically,” he commented. “I think it is reasonable to conclude that the stepwise provisional strategy should remain the approach of choice for the majority of the left main bifurcation interventions.”
Another important issue in this discussion, however, is who should be doing these procedures and how many they need to be doing to be proficient. Data published last year show that operator volume is an important factor in determining outcome, with the lower threshold for improved survival being 16 cases or more per year.
“I think most people would agree that operators should not be doing two or three of these cases per year,” Mamas said. “In [EBC MAIN] there were no requirements for left main case volume, unlike in DKCRUSH, where there were requirements. Given the relationship of volume to outcomes, it’s clear that operator experience really does matter.”
Following the presentation, many took to Twitter to discuss the trial results:
Agree w @twj1974
— MIЯVΛƬ (@mirvatalasnag) May 18, 2021
Provisional isn't necessarily the default based on EBC Main..It is a good place to start, but there are complex anatomies that warrant an a priori 2 stent technique (even if step wise)
Provisional is always the way to go! I was convinced and now I am more convinced about it #EuroPCR 2021 @PCRonline
— Salvatore Brugaletta (@sbrugaletta) May 18, 2021
Need to know a bit more about the anatomies enrolled to draw firm conclusions, but seems to add considerable support to a provisional-first approach for many pts. An added benefit of the provisional strategy is that it may make re-treatment simpler/more effective.
— David J. Cohen, MD, MSc (@djc795) May 18, 2021
That's good news. Though some technical details are important esp use of imaging, what techniques were used for two stent strategy, extent of disease into side branch, what criteria were used to warrant SB stenting in provisional strategy
— Ahmed Suliman (@Sudanheartgroup) May 18, 2021
For me it means that if you leave the circumflex compromised but patent you get away with it for the duration of this study! I think such studies miss important subgroups , I take results with an eyeful of salt, will always work on case per case basis , no one size fits all.
— Hany Ragy (@Hragy) May 18, 2021
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Hildick-Smith D, Egred M, Banning A, et al. The European Bifurcation Club Left Main coronary stent study: a randomized comparison of stepwise provisional vs. systematic dual stenting strategies (EBC MAIN). Eur Heart Journal. 2021;Epub ahead of print.
Disclosures
- EBC MAIN was funded by a grant from Medronic.
- Hildick-Smith reports proctor/advisory fees from Boston, Abbott, Medtronic, Terumo, Edwards, Occlutech, and Gore.
- Lassen reports lecturing and honoraria for Medtronic, Boston Scientific, Biotronik, and Biosensors.
- Stankovic reports no relevant conflicts of interest.



Comments