RACE 3: Effects Wane for Targeted Therapy in Early AF, HF
Patients who received enhanced treatment were no more likely to be in sinus rhythm at 5 years, in contrast to the 1-year results.
The initial benefits of using more-targeted treatments in addition to conventional, guideline-directed medical therapy in patients with early atrial fibrillation (AF) and heart failure fade over time, longer-term follow-up of the RACE 3 trial shows.
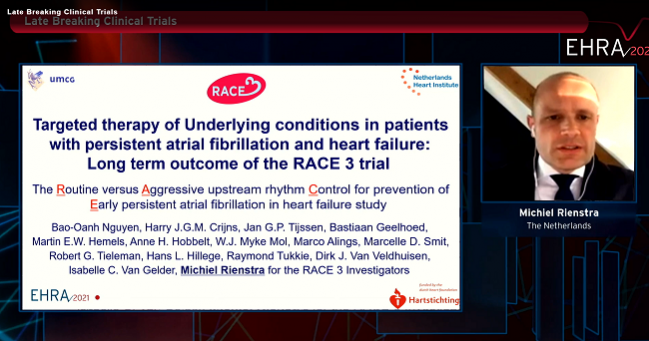
Counter to the 1-year results, patients who received targeted therapy were not more likely to be in sinus rhythm at 5 years than those who received standard treatment alone (46% vs 39%; P = 0.346), according to Michiel Rienstra, MD, PhD (University Medical Center Groningen, the Netherlands).
The rate of composite CV morbidity and mortality—the secondary endpoint—was about 16%, with no difference between trial arms, he reported last week during the virtual European Heart Rhythm Association Congress 2021.
“The RACE 3 study demonstrates that in patients with persistent atrial fibrillation and heart failure, targeted therapies on top of conventional therapy do not improve maintenance of sinus rhythm at 5 years of follow-up,” Rienstra concluded.
The RACE 3 Trial
The idea leading to RACE 3 was that using targeted therapies geared toward modifying the atrial substrate, improving risk factors, and treating diseases underlying AF early on in the disease course would prevent progression and better maintain sinus rhythm. It was thought that that would lessen AF-related symptoms.
The trial, conducted at 14 sites in the Netherlands and three in the United Kingdom, tested that concept in patients with early persistent AF and heart failure. Patients were randomized to conventional AF and heart failure therapy or to conventional therapy plus more-targeted treatments, which included mineralocorticoid receptor antagonists, statins, ACE inhibitors/ARBs, and cardiac rehabilitation. After randomization, all patients underwent electrical cardioversion.
The 1-year results, published about 3 years ago, showed that the addition of targeted therapy boosted the proportion of patients who were in sinus rhythm (75% vs 63%; P = 0.042).
The take-home message for the audience today is: when we treat patients with AF, all risk factors need to be targeted for best results. Dennis Lau
The investigators followed patients for another 4 years to evaluate the longer-term results. Five-year follow-up included data on 107 patients in the targeted-therapy group and 109 in the conventional-therapy group; overall, the mean age of the patients was 64, and 79% were men. Median duration of AF and heart failure at baseline was short at just 2 to 3 months.
The rate of sinus rhythm was assessed using 7-day Holter monitoring, which revealed no difference in the proportion of patients achieving that goal at 5 years.
Changes in some risk factors, like systolic BP and total and LDL cholesterol, favored targeted therapy, whereas there were no between-group differences for others. Diastolic BP and NT-proBNP levels declined to a similar extent in both arms, with body mass index (BMI) seeing a slight uptick. There were increases in left atrial volume and LVEF in both groups.
Managing AF Is ‘Labor-intensive’
Commenting on the results after Rienstra’s presentation, Dennis Lau, MBBS, PhD (Royal Adelaide Hospital, University of Adelaide, Australia), pointed to multiple issues that need to be considered when looking at the waning of the benefits over time.
First, not all risk factors were targeted by the intervention, Lau said, noting the increase in BMI over the course of the trial, as well as the lack of any mention of sleep apnea status or management of alcohol consumption. And second, the intensity and frequency of follow-up lessened in both groups after the initial 12 months.
“So that means that when patients [did] not meet their targets, there was no flexibility for the investigators to escalate intensity of follow-up, as what we would in normal clinical practice,” Lau said.
Additionally, it’s not clear that performing periodic follow-up via telephone is ideal, he commented. “While during this pandemic telehealth is useful, we have found in our experience in our risk factor clinics that this is quite limited,” he said, noting that various measurements—body weight, waist circumference, and BP, for example—cannot be taken. Patient engagement takes a hit with telehealth appointments as well, Lau added.
And finally, Lau said, it’s not clear whether the results would have been similar if the rate of sinus rhythm was evaluated using continuous monitoring with a loop recorder rather than with a 7-day Holter monitor.
“So the take-home message for the audience today is: when we treat patients with AF, all risk factors need to be targeted for best results,” Lau stressed. “And secondly, managing AF is labor-intensive, and we need specialized AF clinics for successful treatment to provide integrated care to maximize patient engagement.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Rienstra M. Targeted therapy of underlying conditions in patients with persistent atrial fibrillation and mild to moderate stable heart failure: long term outcome of the RACE 3 trial. Presented at: EHRA 2021. April 23, 2021.
Disclosures
- The study was supported by the Netherlands Heart Foundation and the Netherlands Heart Institute. The trial was funded by unrestricted grants from AstraZeneca, Bayer, Biotronik, Boehringer-Ingelheim, Boston Scientific, Medtronic, Sanofi-Aventis, and St. Jude Medical paid to the Netherlands Heart Institute.





Comments