Risk Factor Control Worse in Women Than Men in ISCHEMIA Trial
Though clinical outcomes were no different between sexes, there remains an opportunity for more-equitable treatment.

In the ISCHEMIA trial, women with chronic coronary disease received less-intense guideline-directed medical therapy (GDMT) overall compared with men and were thus less likely to achieve various goals for risk factor control, researchers report.
Women also had lower rates of revascularization that could be explained by lower rates of obstructive CAD on angiography, but clinical outcomes were no different between sexes, according to researchers led by Harmony Reynolds, MD (NYU Langone Health, New York, NY).
It was surprising that female patients were treated less aggressively with medical therapy in the context of the trial, which had algorithms for each treatment target in the protocol and included some monitoring of site performance during the study, Reynolds told TCTMD. “I would not have expected to see goal attainment be so different.”
She noted, however, that the undertreatment of women with coronary disease is a “known phenomenon” that has been seen in prior studies, including other clinical trials. And it doesn’t appear to be related to poorer medication adherence in women. Although women had slightly worse adherence in the ISCHEMIA trial, the difference compared with men was not that great, she said.
“I have to assume that there’s some kind of implicit bias. I can’t rule out, of course, that the women want less-intensive therapy, but I have a feeling that this relates to implicit bias among physicians [who think] that women are at lower risk,” Reynolds said. “As we show in this paper, women are not at lower risk. Maybe they should be if they’re treated as aggressively as men, but they aren’t at lower risk.”
The findings, published online this week in the Journal of the American Heart Association, provide “one more reminder that we need to force ourselves to be attentive to medical therapy goals at every visit for every patient,” Reynolds said. “We need to be more attentive to making sure that all our patients are getting the same aggressive medical therapy for coronary artery disease. We know medical therapy works, and we need to apply it rigorously.”
Sex Differences in Chronic Coronary Disease
Women with chronic coronary disease are generally older with more comorbidities and less obstructive CAD than their male counterparts. Prior studies have shown that their risk of adverse cardiovascular outcomes is similar, however.
Previous research also has demonstrated that women with chronic coronary disease are less likely to undergo revascularization than are men, and may have poorer outcomes when they do get revascularized. It’s unclear how much of this treatment disparity can be traced to differences in ischemia severity between sexes and, in the clinical trial setting, whether protocolized care may impact the gaps in use of revascularization or GDMT.
To explore these issues, Reynolds et al delved into the ISCHEMIA trial, which included 5,179 patients (median age 64 years; 22.6% women) with chronic coronary disease, preserved ejection fraction, and moderate-to-severe ischemia on stress testing randomized to an initial invasive strategy or conservative management. The main results showed that the risk of adverse cardiovascular outcomes didn’t differ between strategies.
We need to be more attentive to making sure that all our patients are getting the same aggressive medical therapy for coronary artery disease. Harmony Reynolds
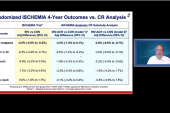
The current analysis highlights some key differences between men and women in the trial. In the invasive arm, women and men were equally like to undergo catheterization, although women had a lower rate of revascularization at any point during follow-up (73.4% vs 81.2%; P < 0.001). That can be tied to a lower severity of coronary disease among women, who were more likely to have no stenosis ≥ 50% on angiography (12.3% vs 4.5%) and less likely to multivessel (60.0% vs 74.8%) or three-vessel disease (29.8% vs 42.7%; P < 0.001 for all) compared with men.
Catheterization rates also were similar by sex in the conservative arm of the trial. Revascularization rates didn’t differ between women and men overall in this group, but among the subset who underwent catheterization, revascularization was less frequent in women (72.3% vs 82.3%; P = 0.007).
As seen in prior studies, use of GDMT overall was lower in women than in men, with fewer risk factor goals achieved by the end of the trial. For instance, women were significantly less likely to attain a systolic blood pressure goal < 140 mm Hg (73.6% vs 77.9%) or an LDL cholesterol goal < 70 mg/dL (50.2% vs 61.3%), and to be treated with aspirin or an aspirin alternative (95.6% vs 97.2%), “despite protocolized trial guidance on medical therapy,” Reynolds et al report. Of note, women were less likely than men to be treated with a high-intensity statin (60.7% vs 64.3%; P = 0.025), and had a lower rate of achieving an HbA1c level below 8%, although this was not a specified goal of therapy in the trial.
Women scored lower on a scale of medication adherence than did men, but the difference was not that great, Reynolds said.
“Although we do not have access to detailed information about dose titration in response to blood pressure and laboratory values in the ISCHEMIA trial, analysis of the relationship between risk factor goal attainment and outcomes in the trial is ongoing,” the investigators write. “Nevertheless, the imperative to achieve equitable use of GDMT implementation among women with chronic coronary disease is both an important challenge and an opportunity for improved clinical outcomes.”
Room for Improvement
Despite the suboptimal use of GDMT in women observed in the trial, the rate of the primary endpoint (CV death, MI, or hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest) was no different between the sexes—14.8% in women and 14.3% in men (adjusted HR 0.93; 95% CI 0.77-1.13). There were similar results for other outcomes, with the exception of periprocedural MI, which was less frequent in women (1.0% vs 2.2%; adjusted HR 0.40; 95% CI 0.21-0.76), consistent with lower rates of revascularization.
“It seems like there’s not much going on there, but I think that under the surface, there’s quite a lot going on there because women have less extensive coronary disease, and that is a powerful predictor of outcomes in stable coronary disease and within the ISCHEMIA trial,” Reynolds said. Counterbalancing that lower risk and resulting in comparable outcomes, however, is that women are also older on average, with a higher burden and poorer control of risk factors.
There shouldn’t really be these discrepancies. Eugenia Gianos
Eugenia Gianos, MD (Northwell Health, New York, NY), chair-elect of the American College of Cardiology’s Prevention of Cardiovascular Disease Council, agreed with that assessment, adding that the differences in the intensity of GDMT between the sexes were surprising and disappointing in the context of ISCHEMIA, even if such disparities have been observed in prior studies.
She, too, mentioned the possible impact of bias on the part of treating physicians to explain the findings, but also said it could be that there are differences stemming from patients declining or discontinuing their medications.
Overall, though, “there’s a lot to be figured out still as to why those differences were there,” Gianos said, noting that there was a low proportion of women in the trial and a lack of information on specific drugs or doses used for GDMT.
Nonetheless, “the reality is that nowadays we have all of the therapies needed to get people to goal, so there shouldn’t really be these discrepancies, and maybe we just need more education of providers about potential biases or [about] the barriers faced by patients in terms of adherence and uptake,” Gianos said, calling for additional high-level research focused on sex disparities.
To underscore the importance of medical therapy in chronic coronary disease, Reynolds alluded to the treatment of heart failure with reduced ejection fraction, a field that “is moving towards being more aggressive early and increasing multiple drugs at the same visit with the idea that you will achieve better outcomes if you get to goals faster. Perhaps here it’s the same story—that we need to focus on getting our therapeutic armamentarium implemented and implemented at a level that’s going to be useful right away instead of introducing things step by step.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Reynolds HR, Cyr DD, Bairey Merz CN, et al. Sex differences in revascularization, treatment goals, and outcomes of patients with chronic coronary disease: insights from the ISCHEMIA trial. J Am Heart Assoc. 2024;13:e029850.
Disclosures
- The study was supported by grants from the National Institutes of Health. The project was supported in part by a Clinical Translational Science Award from the National Center for Advancing Translational Sciences.
- Reynolds reports receiving grants from the National Heart, Lung, and Blood Institute during the conduct of the study and support from Abbott Vascular (donation of optical coherence tomography catheters for an unrelated research study) and Biotelemetry Inc (donation of telemetry monitors for an unrelated research study.





Comments