Robotic PCI Can Protect Cath Lab Staff From COVID-19, Small Study Suggests
It remains unclear, however, whether the risk is all that high in the first place when adequate PPE is used.
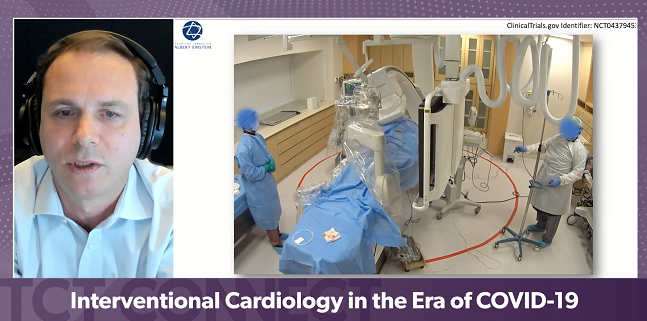
Performing PCI with the assistance of a robotic system may be one way that cardiac cath lab personnel can minimize risks of contracting SARS-CoV-2 and other infectious diseases, a proof-of-concept study conducted during the COVID-19 era shows.
During 10 PCIs, all physicians and other workers managed to remain outside the “spread zone”—which was within 2 meters of the patient’s head—for at least half of the duration of the procedure, Pedro Lemos, MD, PhD (Hospital Israelita Albert Einstein, São Paulo, Brazil), reported last week during the virtual TCT Connect 2020.
The percentage of time spent outside the spread zone ranged from a low of 79.0% for nurses to a high of 96.4% for technicians and anesthesiologists.
All interventions were angiographically successful, and no patients died or had an acute occlusion in the hospital.
Lemos called robotic PCI “a thoughtful strategy” to reduce the proximity of healthcare personnel to potentially infectious patients, but a panel discussion following his presentation focused on whether the risk of infection with SARS-CoV-2 or other respiratory viruses in the cath lab is really all that high to begin with when appropriate precautions are taken.
“It’s an important talk because I think we need to be [cognizant] of the occupational hazards of being in the cath lab, and too often we don’t think about it,” Timothy Henry, MD (The Christ Hospital, Cincinnati, OH), one of the moderators of the session, commented, referring to radiation risks, orthopedic issues, and infections.
But, he asked the other panelists, how big of a problem is the infectious risk? There was extreme concern about dangers to cath lab workers in the early days of the COVID-19 pandemic, when personal protective equipment was in short supply, but based on the panelists’ responses, it doesn’t seem as if SARS-CoV-2 transmission during procedures has been a major problem. “I know lots of interventional cardiologists who caught it from their college kids, but I don’t know anybody that’s caught it that has confirmed transmission in the cath lab,” Henry noted. “With adequate PPE you can take patients to [the] cath lab very safely, and that’s an important message as well.”
Getting Staff Away From the Table
According to the Centers for Disease Control and Prevention, exposure to respiratory droplets containing SARS-CoV-2 produced through exhalation is the primary way that people become infected with the virus.
Cath lab setup has not changed during COVID-19, although all personnel are now wearing more-extensive personal protective equipment [PPE], Lemos noted. For conventional procedures, physicians and other staff must remain right next to the patient—within 1 to 2 meters, the high-risk zone for SARS-CoV-2 spread.
When thinking about the ideal cath lab setup that takes into consideration interpersonal air exposure during a situation like COVID-19, Lemos said, “the idea is to have less people in the room, and for those still in the room, the ideal would be [to] stay away from the patient at least 2 meters and that’s only possible if you use robotic PCI.”
At his center, that’s done using the CorPath GRX system (Corindus), which enables the manipulation of guidewires, guide catheters, and rapid-exchange devices, all controlled by a physician sitting at a control cockpit outside of the cath lab.
Lemos and his colleagues designed a feasibility study—called Robot-Air—to evaluate the use of robotic PCI as a strategy to reduce risks from SARS-CoV-2 and other respiratory viruses. It included 10 patients (mean age 60.2; 90% men) with 16 total lesions. It was a high-risk population, Lemos said, since all but one patient had NSTEMI and half had diabetes. Operators used an average of two stents, with a mean procedure duration of 77 minutes. On the lesion level, 87.5% of interventions were done entirely using the robotic system. For the remaining 12.5%, at least one interventional step was done manually.
The primary endpoint was a composite of angiographic success; the ability to keep the cath lab team positioned more than 2 meters away from the patient for at least half the duration of the procedure; and no fatal events or acute occlusions in the hospital. This was achieved in all cases.
To assess the time various team members spent outside the “spread zone,” the researchers filmed all procedures using an overhead camera and marked off a circle measuring 4 meters in diameter on the floor. The patient’s head was centered within the circle. Cath lab personnel were trained to stay out of the circle as much as possible.
All personnel, including senior physicians, fellows, nurses, technicians, and anesthesiologists, spent at least 50% of the procedure outside of the spread zone. For the whole team, the average proportion of time spent outside the area was 90.1%.
‘An Allegory for What May Be Coming in the Future’
After the presentation, Sahil Parikh, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), one of the moderators of the session, said the study is “a good demonstration of how robotic PCI can preserve us from not just the risks of radiation but also from infection.” One of the challenges, however, is that penetration of robotic PCI is limited around the world because few cath labs have the system and proficiency with it, he said. He asked Lemos whether he’d consider using this approach in emergency situations.
Lemos responded that all patients in this study were “semi-elective,” with no STEMI cases. The next stage for robotic PCI will be evaluating it in situations where speed is critical, he said. “Right now, we should keep robotic PCI for semi-elective and elective procedures, especially for those procedures where you, upfront, think that exposure to radiation and [the time spent] being close to the patient will be long.”
Discussant Mamas Mamas, BMBCh, DPhil (Keele University, Stoke-on-Trent, England), commented that Robot-Air is “a really interesting proof-of-concept study,” but he pointed out that at his high-volume PCI center, there has not been a single case of COVID-19 spread in the cath lab.
There are two things to keep in mind, Mamas said: robotic PCI does not isolate operators from patients and elective PCI should not be performed during a situation like COVID-19. “Elective PCI does not prolong life, [and] does not reduce risk of AMI. We should not be doing elective cases during this period, particularly at the peak of the pandemic,” he said.
After Henry pointed at that it’s been shown that patients can be brought to the cath lab safely with adequate PPE, Parikh noted that the current COVID-19 situation in New York City is much different than it was back in the difficult days of March and April. “While I agree there have not been issues with PPE now, there were definitely times where we didn’t know what the right PPE is, and I think that this study by Dr. Lemos and his colleagues may be an allegory for what may be coming in the future,” he said, adding that many people remember the preparations that were made for a potential Ebola outbreak that fortunately never manifested. “I think the proof of concept is still important.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lemos PA. Robot-assisted PCI as a strategy to reduce the risk of intra-procedure contamination by COVID-19 and other respiratory viruses. Presented at: TCT 2020. October 14, 2020.
Disclosures
- Lemos and Henry report no relevant conflicts of interest.
- Parikh reports institutional grant support/research contracts from Shockwave Medical, TriReme Medical, Surmodics, and Abbott Vascular; personal fees from Abiomed, and Terumo Medical Corporation; and honoraria or fees for consulting or speaking to his institution from Boston Scientific, Medtronic, CSI, and Philips.
- Mamas reports institutional grant support/research contracts from Abbott Vascular, Medtronic, and Terumo and personal fees from Terumo and Daiichi-Sankyo/Eli Lilly.


Comments