Seeing Is Believing: Experts Predict an Expanded Role for Cardiac CT in Structural Interventions
Cardiac CT in aortic, mitral, tricuspid, and pulmonary valve procedures, not to mention the LAA, can make procedures safer and potentially more durable.
WASHINGTON, DC—Multiple roles for cardiac CT have become ingrained in the everyday practice of structural interventionalists, but still more are emerging as the field evolves, according to cardiac imaging specialists gathered here at the Society of Cardiovascular Computed Tomography 2017 Annual Scientific Meeting.
The simple fact that the devices that structuralists work with today are different than even a few years ago—and will continue to see rapid change—poses a challenge for those dedicated to capturing images before, during, and after the procedures.
But staying updated on the advances of cardiac CT is essential for imagers, clinicians, and researchers alike, Gary Mintz, MD (Cardiovascular Research Foundation, New York), who co-chaired the session, told TCTMD. While updates on uses of CT in TAVR are the most “clinically relevant” today given how routine aortic valve interventions have become, he said, other information presented in the session relating to mitral, left atrial appendage (LAA), and tricuspid arenas “can help guide therapy [and] design devices.”
Many Roles for CT in TAVR
Jonathon Leipsic, MD (St. Paul’s Hospital, Vancouver, Canada), reviewed the many advantages of CT in TAVR, noting that while CT’s role is this arena is well-established, “we need to still move forward with the integration of imaging almost more than ever to help improve clinical outcomes,” he said. “This is because of course now that we're performing TAVR in intermediate- and low-risk populations, the room for error and complications is totally absent.”
Among many tasks CT can help with is in clarifying valve morphology in complex cases, Leipsic explained. “That’s something that we in CT took a back seat on for too long,” he said, adding that this is important because younger patients tend to exhibit “more unusual morphologies.”
There is also a need for developing better sizing algorithms for TAVR. “We clearly need to do better, [and] we need to push CT,” Leipsic said. Even though CT has been used for valve sizing for many years now and is credited with reducing rates of paravalvular leak, “the reality is that one size cannot fit all.” With an ever-growing number of TAVR devices on the market, “we need to define sizing algorithms that are device specific,” he said.
Additionally, CT can help with the increasing number of valve-in-valve procedures being performed, Leipsic commented. “If you’re imaging someone for aortic valve-in-valve, you have to understand the potential risks that come from the procedure,” he said. “The one that's most feared that can be prevented with CT is coronary occlusion, but to prevent coronary occlusion you have to understand the mechanism.”
He explained that since the aortic valve is “flipped up” in native TAVR—and this is not the case when a patient already has a surgical valve in place that is kept open—positioning and sizing is critical.
Finally, CT can also be used for thrombus detection. Leaflet thickening occurs in about 10% of patients after both TAVR and surgical AVR, Leipsic said, and although it appears to resolve with anticoagulation, whether—and how—it should be treated remains unclear.
“There may be a signal of a connection between early leaflet thickening, early valve thrombus formation, and mechanisms for early valve degeneration,” Leipsic said, but all of these questions will need to be answered by ongoing studies. Whether CT should be used more routinely to follow patients for this potential complication also remains contentious.
Moving Into Mitral
In a second presentation, Leipsic discussed about CT’s role in mitral valve procedures, citing five ways this imaging modality can help:
· Anatomic assessment of valvular apparatus
· Help with annular sizing and device selection
· Understanding mechanisms and risk of LVOT obstruction
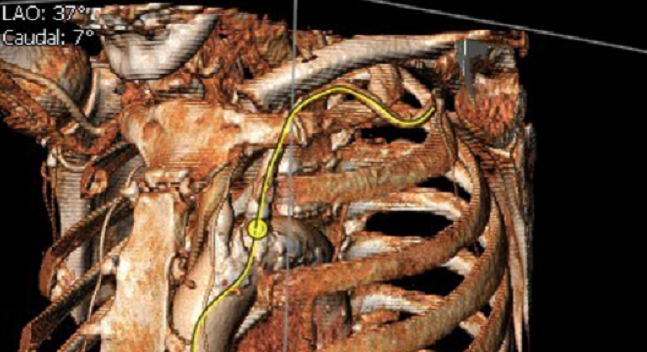
· Prediction of appropriate fluoroscopy angles for coaxial deployment
· Help with access point localization
“We know that the mitral valve is much more complicated than the aortic valve,” he said. “When we interrogate the mitral valve, we need to look at things like areas of infarction, we need to look at the chordal anatomy, the papillary leaflet interaction, and the network that forms the mitral apparatus. We can do that in a stepwise fashion, . . . [and] it helps when the image quality is this nice.”
One of the main “pitfalls” of CT in the mitral space has been overdiagnosis of mitral valve prolapse, Leipsic acknowledged. “Overdiagnosis has long been the bane of computed tomography in other parts of the body, so we need to make sure that we don't do it in the mitral valve.”
For transcatheter aortic valve procedures, CT allows for “granular evaluation” of the annulus size; the same level of confidence is needed in mitral procedures, Leipsic said. But “accuracy is impossible without reproducibility,” he claimed. “What I've learned a lot through working with cardiologists is that what really matters is predicting risk for the patient.” As such, what’s needed is a standardized way to measure the mitral annulus by CT that is going to inform the decision-making by proceduralists, “and I can't do that if our measurements are all over the map,” he said.
Overdiagnosis has long been the bane of [CT] in other parts of the body, so we need to make sure that we don't do it in the mitral valve. Jonathon Leipsic
Leipsic’s team now uses software systems that allow for “fairly standardized, reproducible measurements of the mitral annulus” that can be attained in a stepwise fashion. This is also important, because of the diversity of mitral devices in the pipeline today, he said. “We need to help the proceduralists understand whether the patient’s specific anatomy is suited to that device.”
After Leipsic’s presentation, Mintz stressed that “the one thing that has not been addressed is the importance of assessing the peripheral vasculatures of all these procedures. Those of you who are not interventionalists have to understand these catheter-based valves [and] delivery systems are very, very large,” he said. So “knowing the status of the vasculature is critical.”
Mintz also pointed out that while there are so many mitral replacement devices under investigation, they have a long way to go in terms of proving their safety and efficacy. “None of them may survive [to market], which is also reality,” he commented.
Co-chair James K. Min, MD (Weill Cornell Medical College, New York), agreed. “In the transcatheter mitral valve replacement space, there are so many different valves at this point in time and we don't know which, if any, are going to be successful on a routine basis,” he said. “But given their morphology and their sizing and their shapes and the way they're delivered, I don’t think there’s going to be [only] one way to measure the mitral valve on CT.”
Other Roles for CT: LAA Occlusion
Next up, Omar Khalique, MD (Columbia University Medical Center, New York), walked the audience through CT’s role in LAA occlusion for stroke prevention, noting that while the Watchman (Boston Scientific) is the only device currently available in the United States, “there are going to be others . . . so we have to learn how to image these.”
The objectives of preprocedural imaging for LAA closure are to rule out thrombus, assess the anchoring zone dimensions for device placement, assess other structures in the LAA which may interfere with device placement, and identify the transseptal puncture site, he said.
While transesophageal echocardiography (TEE) is often seen as the gold standard for LAA procedures, it may not be the best modality for thrombus identification. And the lesson learned from TAVR, where CT has supplanted echocardiography, is that “3-D imaging is better than 2-D,” he said.
The key message is that 3-D imaging is needed. Omar Khalique
CT may also help to improve on clinical results, Khalique noted, citing the PROTECT-AF study. “Although the clinical results are good in the short- to medium-term, here we see that 32% of patients in the trial had some degree of peri-device flow at 12 months. I don't know what this means in the long-term, but I can presume some of this is due to these 2-D measurements that are being performed, and we saw this early on in the TAVR space as well.
“The key message is that 3-D imaging is needed,” he said.
In the future, CT can also be used for complete access planning, overlay/fusion imaging, and to create 3-D printed models, Khalique predicted, stressing that the images will have to be acquired “appropriately” with proper protocols in place.
Even today, Khalique believes CT could play a bigger role in LAA occlusion procedures. “I’m not in charge yet,” Khalique quipped, “but if I was, I would do a preprocedural CT on the majority of these patients with a delayed scan for thrombus rule out, and then I would perform a TEE prior to the invasive procedure if a thrombus diagnosis was unclear, which would be in the minority of cases if the protocols are followed. Lastly, I would do intraprocedural TEE for guidance.”
Useful in the ‘Forgotten’ Valves
Finally, Subhi Al’Aref, MD (Weill Cornell Medicine, New York), reviewed the advantages of CT imaging in understanding the morphology of the “forgotten” tricuspid and pulmonary valves, particularly in patients with complex anatomy and other underlying diseases.
CT is the “gold standard imaging modality for assessment of calcification,” said Al’Aref, and is “also useful for assessment of the relationship between the RCA and tricuspid valve annulus.”
Imaging is absolutely essential for safe and efficacious delivery of percutaneous therapies, especially when surveying right-sided structures. Subhi Al’Aref
With 3-D printing being used more, CT also has the potential to aid operators in providing tangible models of patient specific anatomy that can help with procedural planning and device sizing, he added.
Looking forward, better incorporating CT into both tricuspid and pulmonary valve interventions could “lead to better safety and efficacy of percutaneous therapy and improved outcomes,” he concluded. “So the take home message from this presentation is that imaging is absolutely essential for safe and efficacious delivery of percutaneous therapies, especially when surveying right-sided structures.”
Photo Credit: Remi Kouz
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Leipsic J. CT for TAVR: What have we learned? Presented at: SCCT 2017. July 7, 2017. Washington, DC.
Leipsic J. MDCT to guide mitral valve interventions. Presented at: SCCT 2017. July 7, 2017. Washington, DC.
Khalique O. LAA closure: a role for CT or is TEE all you need? Presented at: SCCT 2017. July 7, 2017. Washington, DC.
Al’Aref S. Tricuspid and pulmonary valve transcatheter interventions. Presented at: SCCT 2017. July 7, 2017. Washington, DC.
Disclosures
- Leipsic reports serving on the speakers bureau for GE Healthcare and Edwards Lifesciences; receiving grant support from CIHR, NIH, GE Healthcare, and Heartflow; serving as a consultant to Heartflow, Philips, Samsung, Edwards Lifesciences, Neovasc, Circle CVI, and Valtech; and providing corelab services for NIH, Edwards Lifesciences, Neovasc, Tendyne, Medtronic, and Ancora.
- Khalique reports providing CT core lab services for the aMAZE trial.
- Al’Aref reports no relevant conflicts of interest.


Comments