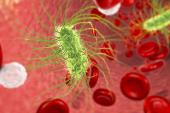
Severe Infections Linked to a Variety of CV Events, Both Acute and Long-term
In the month after a hospital stay for infectious disease, patients had a nearly eightfold increase in MACE risk, UK data show.

(UPDATED) Patients with bacterial or viral infections severe enough to merit hospitalization are at increased risk of experiencing a CV event compared with those who lack an infectious-disease diagnosis, according to an analysis of more than 330,000 participants in the UK Biobank.
Risk related to infection spiked particularly in the first month after the hospital stay, researchers found, but remained significantly higher even a decade later.
“With infectious diseases being common, their contribution to the burden of cardiovascular disease is potentially substantial, yet the proportion of cardiovascular events that could be attributable to all infections is unknown,” Pyry N. Sipilä, MD, PhD (University of Helsinki, Finland), and colleagues write.
Based on their calculations, it turns out severe infections are responsible for around 4% to 6% of major cardiovascular events—which would translate to as many as 150,000 deaths in high-income countries each year, the researchers note. By comparison, diabetes would be expected to account for 3.3% of major cardiovascular events and smoking for 9.7%.
Earlier studies also have illustrated the potential harms of severe infections.
Sipilä, speaking with TCTMD, said that on this backdrop their findings didn’t come as a surprise but did extend the evidence base. “There had been some studies on specific infections, which had shown that pneumonia and influenza and COVID-19 [are] associated with an increased risk of major cardiovascular events,” he noted. “So then we wanted to see if that applies to infections in a broader sense and take a wide look at lots of different infections.”
Behnood Bikdeli, MD (Brigham and Women's Hospital, Boston, MA, and Yale University School of Medicine, New Haven, CT), during the COVID-19 pandemic focused much of his research on the connection between inflammation and cardiovascular disease in infectious disease. What stands out about the current paper, he said, is the breadth of infections it considers and the length of its follow-up.
“I think this was an interesting investigation. It raises the alarm for some things that we’ve overlooked in the past,” he commented to TCTMD. “It builds off of a precedent hypothesis, it is biologically plausible, and they replicated it in several different data sources.”
UK Biobank Data
For their study, published online yesterday in Circulation, researchers analyzed data on 333,683 UK Biobank participants (mean age 56.5 years) who did not have CVD when they enrolled between 2006 and 2010.
Over a mean follow-up of 11.6 years, 54,434 of these individuals were hospitalized for an infection. Most commonly, the infections were of the urinary tract, unspecified gastroenteritis, or unspecified lobar pneumonia. A total of 11,649 UK Biobank participants had major cardiovascular events, amounting to an incidence of 3.0 per 1,000 person-years. More than half of the events (56.1%) were MIs or cardiac deaths, and the rest were fatal or nonfatal strokes.
The participants who’d had an infectious disease were at increased risk, particularly during the first month (HR 7.87; 95% CI 6.36-9.72) but also thereafter (HR 1.47; 95% CI 1.40-1.54). Findings were similar when analyzed in a replication cohort of 271,533 people residing in Finland (mean age 34.4 years), for whom the mean follow-up was 19.2 years. The links were strongest for pneumonia and viral infections, septic (versus nonseptic) infections, recurrent hospitalizations for infection, and among patients with the highest baseline CV risk.
The individual endpoints of death from coronary heart disease or stroke, nonfatal CV event, MI or coronary heart disease death, stroke, ischemic stroke, and hemorrhagic stroke all were elevated after severe infections. After accounting for traditional CV risk factors, all of the relationships were attenuated though still significant.
Being hospitalized for noninfectious causes also increased risk, but only about half as much as did severe infections (HR 3.7 in the UK Biobank within the first month).
What’s the Connection?
Sipilä et al cite several reasons why an infection may lead to cardiovascular events in the short term. “For example, activation of inflammatory molecules and platelets, increased inflammation in atheromatous plaques, endothelial dysfunction, and augmented sympathetic nervous activity with catecholamine release may contribute to electrical instability of the heart, atherosclerotic plaque instability, and a concomitant hypercoagulable state,” they explain, adding that while the risk may linger beyond this acute phase, it makes sense that the risk becomes smaller with time.
Though they didn’t look into those processes in this paper, said Sipilä, “it’s likely there are shared mechanisms” among the different infectious diseases.
For Bikdeli, thromboinflammation is an additional mechanistic pathway worth considering. “When there is infection, there is inflammation and it is true that there is activation of the coagulation cascade: there is a procoagulant profile in these patients,” he observed. Moreover, infections can trigger the release of neutrophil extracellular traps (NETs), meant to defend the body against pathogens but also capable of causing thrombus formation.
Yet confounding might be another reason for these findings, he suggested. “There could also be a difference in case mix, . . . such that people who are more susceptible to having these serious infections might just be sicker than [other] individuals at baseline, [and] by virtue of being sicker they can also have a higher risk of cardiovascular events.”
Bikdeli cautioned, too, using ICD codes to identify both serious infections and CV outcomes could be problematic. While the “signal” of an association is convincing, “I would be very cautious about the point estimates and confidence intervals,” which could be unreliable, he said. As in other studies that use large data sets, “there’s a huge chance that we’re getting a lot of noise and putting it into the signal.”
Even with these caveats, however, “in general the results do make sense,” he said, adding that he hopes future studies use clinical databases or, if they use administrative claims, take steps to validate the data’s accuracy. Only once the association between acute infection and CV events is fully quantified will it be possible to ask what can be done to mitigate the risk, said Bikdeli.
As for what should come next, Sipilä said, “It would be lovely to have clinical studies about people who are hospitalized for infections, so [we could know if] there are any interventions that could be used to reduce their risk of cardiovascular events and if those interventions are safe. But we have population data at our disposal, so at the moment we can’t study that.” Randomized studies would be especially welcome, he added.
For clinicians, the investigators highlight the benefits of using tools like the American College of Cardiology/American Heart Association pooled cohort equations for 10-year atherosclerotic cardiovascular disease risk to identify which patients can benefit from more-intensive care.
“Although particular attention may be required for this group because of their increased risk of infection-related cardiovascular events, treatment decisions must account for the risk of major intracranial and gastrointestinal bleeding, which may also be increased in the acute phase of an infection,” they say. “Avoidance of potential triggers of cardiac and cerebrovascular events during the acute phase, such as excessive use of alcohol, overeating, lack of sleep, work stress, and long working hours, may be beneficial and is without harm.”
Indeed, antithrombotics used to avert blood clots carry the risk of bleeding, as evidenced by the RECOVERY trial of aspirin in COVID-19 patients, Sipilä noted. Given this “delicate” balance, he said, randomized trials are required to look at safety before it’s possible to recommend specific treatment regimens.
Another approach to preventing CV events, he suggested, would be to treat the underlying risk factors, such as high LDL and blood pressure levels.
And of course, preventing infection in the first place would be even better. Bikdeli highlighted a meta-analysis showing that people who get vaccinated against influenza see lower risk of MACE, even more so if they’ve recently had acute coronary syndromes. Sipilä agreed that vaccination would be a “sensible strategy here,” given the very low risk of vaccines and great potential for benefit.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Sipilä PN, Lindbohm JV, Batty GD, et al. Severe infection and risk of cardiovascular disease: a multicohort study. Circulation. 2023;Epub ahead of print.
Disclosures
- This work was funded in whole, or in part, by grants from NordForsk, Academy of Finland, Helsinki Institute of Life Science, Emil Aaltonen Foundation, Finnish Medical Foundation, Päivikki and Sakari Sohlberg Foundation; Finnish Foundation for Cardiovascular Research, US National Institute on Aging, UK Medical Research Council, and Wellcome Trust.
- Sipilä reports grant support during the conduct of the study from NordForsk, Academy of Finland, Helsinki Institute of Life Science, Aaltonen Foundation, and Finnish Medical Foundation.
- Bikdeli is supported by a Career Development Award from the American Heart Association and VIVA Physicians for the PE-EHR+ study, was supported by the Scott Schoen and Nancy Adams IGNITE Award, and is supported by the Mary Ann Tynan Research Scientist award from the Mary Horrigan Connors Center for Women’s Health and Gender Biology at Brigham and Women’s Hospital, and the Heart and Vascular Center Junior Faculty Award from Brigham and Women’s Hospital. He is a consulting expert, on behalf of the plaintiff, for litigation related to two specific brand models of IVC filters.




Comments