Shorter, Lower-Dose Ultrasound-Accelerated Thrombolysis for Acute PE Keeps Early Promise: OPTALYSE PE
New data presented at ISET 2018 show sustained efficacy, low mortality, and improved quality of life at 1 year.
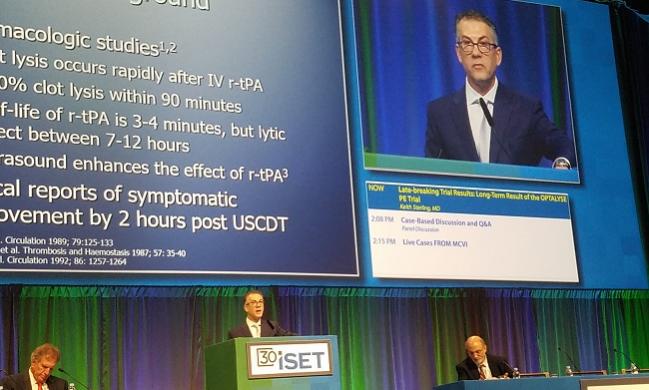
HOLLYWOOD, FL—Even with lower-dose infusions given for short durations, patients with pulmonary embolism (PE) who receive ultrasound-enhanced catheter delivery of recombinant tissue plasminogen activator (r-tPA) continue to do well over the long term, according to new data from the OPTALYSE PE trial presented yesterday at the International Symposium on Endovascular Therapy (ISET) 2018.
In a field where hard evidence is lacking, the findings help fill in pieces of the puzzle over how best to treat PE.
OPTALYSE PE investigators sought to answer two questions, Keith Sterling, MD (Inova Alexandria Hospital, McLean, VA), said in his presentation: “Can we lower the fibrinolytic dose to improve safety without compromising efficacy? Can we improve efficiency and decrease cost by reducing infusion time?”
The trial occurs on the backdrop of two key trials: ULTIMA and SEATTLE II.
ULTIMA confirmed in 2013 that a fixed-dose regimen of ultrasound-assisted catheter-directed thrombolysis using the EkoSonic Endovascular System (BTG) on top of IV heparin was superior to anticoagulation alone in improving RV dysfunction without increasing bleeding complications. Patients in the device arm received a 10-mg r-tPA dose over 15 hours. Then, in 2015, the SEATTLE II trial showed that 24 mg of r-TPA given over 12 or 24 hours decreased the RV:LV ratio by 30%, with reductions in pulmonary hypertension and obstruction. There was no intracerebral hemorrhage, and 10% of patients experienced major bleeding.
EkoSonic received US Food and Drug Administration approval in May 2014 for the treatment of acute PE. Since that time, the SEATTLE II protocol has been widely adopted, Sterling said.
For their study, Sterling and colleagues randomized 101 patients with submassive acute PE who had an RV:LV ratio > 0.9 and were hemodynamically stable to one of four arms with varying treatment durations and tPA infusion rates:
- 2 hours at 2 mg/hour per catheter, for a total dose of 4 or 8 mg
- 4 hours at 1 mg/hour per catheter, for a total dose of 4 or 8 mg
- 6 hours at 1 mg/hour per catheter, for a total dose of 6 or 12 mg
- 6 hours at 2 mg/hour per catheter, for a total dose of 12 or 24 mg
The primary efficacy endpoint was reduction of RV:LV by 0.2 on CT angiography at 48 hours after treatment initiation. Safety was assessed as major bleeding events within 72 hours after treatment began.
By 48 hours there was “significant reversal of RV dysfunction in all four treatment groups regardless of the dose, and this ranged between 23 and 26 percent,” Sterling said.
At 1 year, he continued, “basically all patients had more or less a normal RV to LV ratio of around 0.7 and that was statistically significant,” at P < 0.0001. Yet the mean change in RV systolic pressure did not reach significance in all groups, Sterling noted. “This just shows you that possibly pulmonary artery pressure is not the right endpoint we need to be looking at for these patient treatments.”
Six-minute walk distance at 30 days was sustained in all categories out to 1 year, he reported. PE-specific quality of life—measured via a questionnaire that asked about frequency of complaints, limitations in activities of daily living, work-related problems, social limitations, intensity of complaints, and emotional complaints—also improved significantly over 1 year of follow-up.
Mortality at 1 year was 2%. There were two confirmed cases of recurrent PE and one suspected case.
The “lower-dose, shorter duration appears to be as effective as all the other regimens,” Sterling concluded. Not only does this reassuringly match the efficacy seen with the protocols used in SEATTLE II, he said, there may be the opportunity to shorten treatment duration and avoid a stay in the intensive care unit.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Sterling KM. Long-term results of the OPTALYSE PE trial. Presented at: ISET 2018. February 5, 2018. Hollywood, FL.
Disclosures
- Sterling reports serving as a consultant to Boston Scientific and EKOS/BTG; receiving grant/research support from Angiodynamics, EKOS/BTG, and Penumbra; and serving on the speakers’ bureau of EKOS/BTG.


Comments