Surgical Explant or Redo for TAVI Failures? Some Registry Insights
Investigators caution this is an apples-to-oranges comparison, given the complexity of surgical removal of a failed THV.
CHICAGO, IL—Surgically removing a failed transcatheter heart valve (THV) is associated with a higher risk of death compared with redo TAVI, but the long-term prognosis appears to be similar between the two reintervention approaches, according to results from a large global registry.
Patients undergoing THV explantation had higher in-hospital, 30-day, and 1-year mortality compared with a redo procedure, but most of that risk was observed in the first month. Beyond 30 days, a landmark analysis suggested the death risk is similar between the two procedures, report investigators.
Lead investigator Syed Zaid, MD (Houston Methodist, TX), who presented the results from the EXPLANT-OR-REDO TAVI international registry during a late-breaking clinical trial session at TVT 2022, said the difference in clinical outcomes is likely a reflection of two distinct patient populations.
“One important thing that we do recognize is that the redo TAVR and explant groups are fundamentally different,” said Zaid. “This is in some ways comparing apples to oranges.”
Robert Bonow, MD (Northwestern University Feinberg School of Medicine, Chicago, IL), who moderated the session, agreed with the analogy, but he questioned how heart teams decide which patients they’ll send for a redo TAVI procedure versus those they’ll send to surgery. In response, Michael Reardon, MD (Houston Methodist), said patients are typically only sent to the operating room once they’re no longer a good candidate for TAVI.
“The ones that I tend to get—and I’ve done 26 or 28 of these now—are the ones where we can’t do another TAVR,” said Reardon.
Lifetime Management of TAVI Patients
As TAVI shifts into lower-risk patients, the lifetime management of patients with THVs is becoming an important consideration, and this includes the best way to manage patients if the devices fail. Explantation and redo TAVI are two treatment options, said Zaid, with redo TAVI known to have better 30-day outcomes compared with surgical removal.
To look at clinical outcomes across multiple sites with detailed imaging and procedural data, the researchers turned to the EXPLANT-OR-REDO TAVI registry. From 2009 to 2022, 503 patients from 29 international sites underwent redo TAVI or surgical explantation for THV failure during a subsequent hospital admission. In total, 149 TAVI explants were excluded because the cause of failure was endocarditis, which left 176 patients undergoing redo TAVI and 178 patients who had the THV explanted.
Senior investigator Gilbert Tang, MD, MBA (Icahn School of Medicine at Mount Sinai, New York), said the incidence of aortic-valve reintervention was 0.5% in the registry, which is reassuring. “It could be an underestimation,” Tang told TCTMD. “There are patients from other sites who get referred to the participating centers part of this study who had TAVI elsewhere. We don’t really know the denominator.”
The redo TAVI patients were older and had a higher STS-PROM risk score at the time of the index procedure. More redo TAVI procedures were performed in patients with a balloon-expandable Sapien XT (Edwards Lifesciences) valve, while THV explantation was more often performed in those who’d received the newer Sapien 3 device. There was no difference in the types of reinterventions performed with the different generations of self-expanding valve (CoreValve/Evolut R/Evolut PRO; Medtronic).
In terms of mechanisms, structural valve deterioration was more common in patients undergoing redo TAVI procedures, as was THV thrombosis, than in those undergoing TAVI explant. On the other hand, prosthesis-patient mismatch was greater in those undergoing surgical explantation. Both reintervention groups had similar rates of paravalvular leak and delayed valve migration. The time to reintervention was longer in the redo group compared with the TAVI-explant group (median 43.8 months vs 18.0 months; P < 0.001).
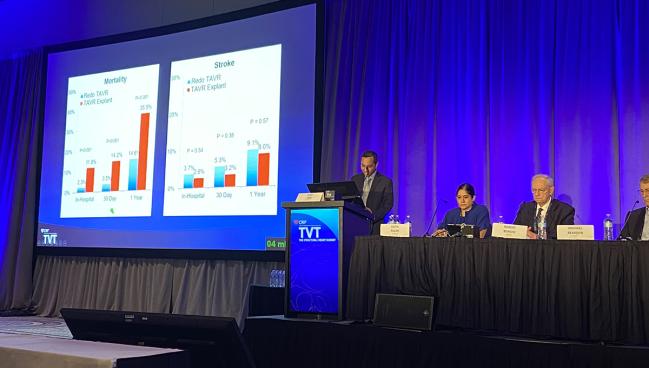
The overall risk of death was significantly higher (P < 0.001) with TAVI explantation compared with redo TAVI:
• In-hospital: 11.8% vs 2.3%
• 30-day: 14.2% vs 3.5%
• 1-year: 35.5% vs 14.6%
In the landmark analysis, mortality beyond 30 days was not significantly different between the two procedures. There was no significant difference in the risk of stroke at any time point. The TAVI-explant group did have longer hospital stays than the redo TAVI group, while vascular complications were more common in the redo group.
The investigators also analyzed mortality differences with the redo and explant reinterventions stratified by the type of THV implanted during the index procedure. They observed no differences in mortality between redo TAVIs performed in balloon-expandable and non-balloon-expandable THVs. Similarly, there was no difference in mortality with explantation based on the type of THV implanted during the index procedure.
Concomitant Procedures With Surgery
To TCTMD, Tang said they aren’t yet sure why there was such a large difference in the time to reintervention with redo TAVI versus explantation. One hypothesis, he said, “is that the patients we need to take to the operating room have other cardiac issues requiring surgery, so why wait?” Also, it’s possible the initial TAVI result was not optimal so the heart team decided to reintervene quicker rather than delay.
“It’s why I think we see the differences,” he said. “It also explains some of the early mortality differences because a good percentage of these [explant] patients had concomitant surgery.”
Anita Asgar, MD (Montreal Heart Institute, Canada), also stressed the differences between the two procedures, noting there were limited data presented on the complexity of the surgical procedure, although such complexity likely explains the difference in early mortality. She noted that 10.7% of patients underwent an aortic root replacement and 15.7% root enlargement.
“There’s morbidity associated with that,” she told TCTMD, noting that these patients were already considered high risk for surgery at the time of the index TAVI. “We have to look to the surgical insult and procedure and why it’s causing that high mortality.”
To TCTMD, Reardon said that TAVI explantation is “not as hard as it’s played out to be” in the hands of experienced operators. Like Asgar noted, the surgery often requires more than explantation. “It’s not that common that we need to do a root replacement,” he said. “We do a lot of annular enlargements now, because if you’re in my operating room and you’re a woman, you never leave with less than a 23-[mm] valve. If you’re a man, you never leave with a less than 25-[mm] valve. If we’re going to operate on you, at least you’re going to get a good heart valve out of it.”
Overall, Reardon believes the number of TAVI explantations will rise in the coming years and said that these cases should be referred to high-volume centers of excellence who have experience taking on such cases.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Zaid S, Goel S, Fukuhara S, et al. Explant versus redo TAVR after TAVR failure: outcomes from the EXPLANTORREDO-TAVR international registry. Presented at: TVT 2022. June 8, 2022. Chicago, IL.
Disclosures
- Zaid and Bonow report no conflicts of interest.
- Tang report consulting/honoraria/speaker’s bureau fees from Abbott Vascular, Medtronic, NeoChord and serving (unpaid) on an advisory board for JenaValve.
- Asgar report grant support/research contract with Abbott Vascular. She reports consulting/honoraria/speaker’s bureau fees from Medtronic, Edwards Lifesciences, and W.L. Gore.
- Reardon reports consulting/honoraria/speaker’s bureau fees from Medtronic, Abbott Vascular, and Boston Scientific.





Comments