TEER Linked to Better 1-Year Survival in Shock Patients With Significant MR
A randomized trial is still warranted in cardiogenic shock complicated by significant MR, but enrollment will be tough.

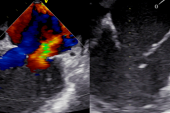
BOSTON, MA—(UPDATED) Among patients with significant mitral regurgitation (MR) and cardiogenic shock, those treated with transcatheter edge-to-edge repair (TEER) are less likely to die or be hospitalized for heart failure at 1 year, according to a large registry analysis.
Compared with prior data in this space—including the IREMMI registry of 93 patients, an observational analysis of 639 patients, and a multicenter patient-level analysis of 141 patients—TEER SHOCK, which was presented today at TCT 2022 and published online simultaneously in the Journal of the American College of Cardiology, is by far the largest single study of TEER in this population with almost 3,800 patients included from the STS/ACC TVT Registry.
With administrative data, “you can't really tell the severity of mitral regurgitation [and] you can't really tell much about cardiogenic shock,” senior author Mohamad Alkhouli, MD (Mayo Clinic, Rochester, MN), told TCTMD. “We don't claim to solve all of those problems, but it is still the largest data set available.”
Even with the 85.6% device success and more than 20% absolute reduction in mortality observed at 1 year following a successful TEER procedure, though, Alkhouli said these results should only be “hypothesis generating.”
Because of the confounders present in a registry study like selection bias, site-reported outcomes, and missing data, he said, “doing a trial is still the right thing to do in my opinion.” The ongoing CAPITOL MINOS trial, which will randomize 144 patients with Society for Cardiovascular Angiography and Intervention (SCAI) class C or D cardiogenic shock and at least 3+ MR to TEER or medical therapy alone, “will be tough to enroll but if they are able to complete it that, [it] would seal the deal.”
In my personal experience, although it's relatively low, I do think this is an excellent solution for patients in shock who’ve got significant mitral regurgitation. Mohamad Alkhouli
To TCTMD, Neil Fam, MD, MSc (St. Michael's Hospital, Toronto, Canada), who is on the steering committee for CAPITOL MINOS, agreed the trial will “probably take a lot of time to enroll enough patients. But if the effect size is the same, maybe the trial will be done earlier than we think, and if enough events accrue, then the DSMB of the trial will end it early.”
Lower Mortality With TEER
For the study, lead author Trevor Simard, MD (Mayo Clinic, Rochester, MN), Alkhouli, and colleagues included 3,797 patients (mean age 73; 59.5% male) from the STS/TVT registry with cardiogenic shock—defined as cardiogenic shock on the data collection form, inotrope use, or mechanical circulatory support—who underwent TEER between November 2013 and December 2021.
Overall, 73% met one criterion for cardiogenic shock, while 18.9% met two and 8% met all three. The STS predicted risk of mortality for mitral valve repair was 14.9%. MR etiology overall was 53.4% degenerative, 27.5% functional, 13.6% mixed, and 5.4% other. More than one clip was implanted in 47.8% of patients. Procedural complications were minor and included VARC major bleeding (3.6%), stroke (1.6%), single-leaflet device attachment (1.3%), and conversion to surgery (0.6%).
Device success—defined as final MR grade < 2+ (88.2%) and MR reduction > 1 absolute grade (91.4%)—was achieved in 85.6% of the total cohort. Those with device failure had a similar risk profile as those with device success (14.8% vs 15.0%) but were generally older, had a higher prevalence of diabetes and chronic obstructive lung disease, and more degenerative MR. Patients in the device failure group also had slightly higher LVEF (42.9% vs 40.7%) and a lower prevalence of moderate-severe or severe MR (84.9% vs 96.1%).
For those with device failure, in-hospital mortality was higher (16.4% vs 9.1%) and length of stay was longer (14.3 vs 12.2 days) compared with those who had device success (P < 0.001 for both). The STS expected-versus-observed 30-day mortality rates in those with device failure showed similar outcomes (15.0% vs 23.0%; O/E ratio 1.53), but in patients with device success, the researchers found lower 30-day mortality compared to the STS expected rates (14.9% vs 13.1%; O/E ratio 0.88).
The risk of all-cause mortality at 1 year was halved in the device success versus failure groups (34.6% vs 55.5%; adjusted HR 0.49; 95% CI 0.41-0.59; NNT 4.8), as was mortality or heart failure admission (29.6% vs 45.2%; adjusted HR 0.51; 95% CI 0.42-0.62).
There were no significant interactions noted between the definition of cardiogenic shock used in the study, MR etiologies, LVEF, and ACS and the interplay between device success and mortality outcomes. Also, a sensitivity analysis looking at the effect of surgical conversion on device success showed no impact.
Alkhouli said he was not surprised by any of the results as they “mimic” what has been seen in patient-level data. While the mortality risk remains high even with a successful TEER, emphasizing the severe illness of the patient population, there isn’t much to lose with sending these patients for this procedure since complication rates were comparable with even other MitraClip populations. “If you're successful in doing the procedure, they still had the mortality similar to what the STS predicted,” he said. “It is a high-risk population, so we could talk about utility/futility, but there was a very strong signal that mortality was lower.”
Calling the difference in mortality observed with successful procedures “extraordinary” despite all the potential confounders, Patrick T. O’Gara, MD (Brigham and Women’s Hospital, Boston, MA), asked in a press conference: “What else do you worry about when you see a 50% reduction in relative risk with a single intervention?”
Also during the press conference, Robert Cubeddu, MD (NCH Heart Institute, Naples, FL), called the data “incredibly reassuring.”
“I want to believe that several of the patients in this registry are patients that I did,” he said. “It is incredibly rewarding to see the results of MR and how that impacts hemodynamics immediately. In my personal experience, although it's relatively low, I do think this is an excellent solution for patients in shock who’ve got significant mitral regurgitation.”
“Our experience,” Fam said, “has been exactly the same as what was reported here, so it's gratifying to see them report these outcomes in such a large data set. The power of it is the sample size and the fact that it's reproducible in so many centers. I think that suggests that it's real.”
Look for MR
The results stress the importance of clinicians being “a little bit more liberal in targeting these patients,” Alkhouli added.
Fam agreed. “The most important thing is that they have to look for MR and then treat it,” he said. “If don't look for it, you can't treat it, and I honestly think not everyone is thinking along these lines and don't realize the MR itself is a target and it can help to get that patient to turn the corner. Obviously, [TEER is] not going to save them all, but it's a very useful adjunct to all the other therapies that patients currently get, and it's not surgery. It's a very safe transvenous procedure that has a low complication rate.”
But while the technical aspects are not that different in performing an elective TEER procedure compared with one in a patient in cardiogenic shock, Alkhouli said “the team and pre- and post- aspects are different because now we're talking about inotropes, observation, CCU, and all of that which we're not used to doing in the elective clip cases. So I think this is more of like a shock team approach that will be new and that will have a learning curve and nuances based on the institution.”
The power of [the outcome] is the sample size and the fact that it's reproducible in so many centers. I think that suggests that it's real. Neil Fam
A shock team might be helpful as is ICU expertise to manage the patient, Fam said, “but like everything in cardiology, early diagnosis and treatment is really what makes the difference. I think just having an expert heart team with people who understand the mitral valve is key.”
But when to decide to send this kind of a patient for TEER will remain a challenge, given the other options many physicians tend to try first, said Susheel Kodali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY),in a discussion following the session. “Part of the interesting thing is the delay to treatment," he said, noting that there was a mean 5.6 day time from hospital admission to TEER in this study. "Is this an upfront therapy in these patients? Probably not. When do you pull the trigger in these patients is the big question."
Effects on CAPITOL MINOS
The big issue that faces the CAPITOL MINOS trial is whether cardiologists will be willing to randomize their patients at this point, Fam said. “I actually think many will be because to this day, many cardiologists and surgeons remain somewhat uncertain or skeptical about what MitraClip can do or TEER in general, but anyone who's had their patients treated and salvaged immediately becomes a convert.”
Because the COAPT trial was “very positive” and MITRA-FR wasn't, “that created a little bit of uncertainty in the hearts of our community,” he continued. “Some heart failure doctors believe it very strongly and use MitraClip as a tool in their practice and it's in the guidelines, but not all. This is all the issue of knowledge translation, and that takes years, sometimes decades, to really make it into practice.”
Anita Asgar, MD (Montreal Heart Institute, Canada), during the trial discussion, said she would have “challenges” randomizing patients to this kind of a trial. “I don’t know if that’s ethical,” she said.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Simard T, Vemulapalli S, Jung RG, et al. Transcatheter edge-to-edge repair in patients with severe mitral regurgitation and cardiogenic shock. J Am Coll Cardiol. 2022;Epub ahead of print.
Disclosures
- Alkhouli reports receiving grant/research support from Boston Scientific and Philips and consulting fees from Abbott, Biosense Webster, Philips, and Boston Scientific.
- Simard and Fam report no relevant conflicts of interest.



Comments