TESLA Falls Short, but Experts Still See Role for EVT in Large-Core Strokes
The totality of the evidence, including from three prior trials, points toward greater use of thrombectomy in this population.

MUNICH, Germany—The latest trial of endovascular therapy (EVT) for large-core ischemic strokes, TESLA, fell short of its primary endpoint. But the totality of the evidence—bolstered by a new patient-level meta-analysis of three prior trials—suggests that the use of thrombectomy will be growing in this setting, experts say.
By the TESLA trial design, to declare the success of EVT plus medical therapy over medical therapy alone in terms of 90-day functional outcomes, the Bayesian prespecified probability of superiority had to exceed 0.975. Although patients treated with thrombectomy tended to do better, the probability of superiority reached just 0.957, Albert Yoo, MD, PhD (Texas Stroke Institute, Plano, TX), and Osama Zaidat, MD (Mercy Health, Toledo, OH), reported last week at the European Stroke Organisation Conference (ESOC).
Some secondary endpoints, as well as an analysis restricted to core-lab imaging reads, however, suggested a benefit of EVT. Moreover, there were no major safety concerns in terms of mortality or symptomatic intracranial hemorrhage (ICH), Zaidat said.
The missed primary endpoint stands in contrast to the findings of three prior trials—RESCUE-Japan LIMIT, SELECT2, and ANGEL-ASPECT—that yielded positive results in patients with an Alberta Stroke Program Early CT Score (ASPECTS) < 6, who were excluded from the initial paradigm-shifting trials that established thrombectomy as a highly effective treatment for acute ischemic stroke.
Amrou Sarraj, MD (University Hospitals Cleveland Medical Center – Case Western Reserve University, OH), who presented a pooled, patient-level analysis of those three prior trials immediately after the TESLA presentation, said his team looks forward to adding data from this fourth trial to the meta-analysis.
But, despite the missed primary endpoint, “I only perceive the results of TESLA as positive,” he said. “They show treatment effect in the same direction” as what was seen in the other three studies.
As for the clinical implications, Sarraj said, “There is no going back. We showed the evidence, we showed the signal. These patients are more likely to benefit with thrombectomy. The safety is very reassuring. We should capitalize [on] this together to expand the treatment, and we really look forward to the guidelines changing sooner rather than later.”
Mitchell Elkind, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), a past president of the American Heart Association, also put the TESLA results into the context of the other trials.
“I tend to look at the evidence in totality, and I think that in combination with those other trials, there’s probably a strong signal that we can be treating people with larger strokes, and I think that’s really exciting,” he commented to TCTMD.
The TESLA Trial
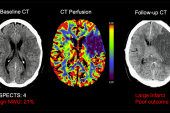
An important consideration when interpreting the large-core trials, Yoo said, is that the various imaging modalities used to assess the size of the infarct differ in sensitivity and specificity. Of note, MRI was used in 86.2% of patients in RESCUE-Japan LIMIT, CT perfusion was used in all patients in ANGEL-ASPECT, and CT perfusion was used in nearly all patients in SELECT2, with MRI employed in a small proportion. All of those trials, Yoo said, restricted inclusion to patients with ASPECTS of 3 to 5.
In TESLA, the investigators aimed to identify patients with large ischemic cores using only noncontrast CT (NCCT), which is available in all stroke centers and thus more accessible than more-advanced imaging modalities. They also included patients with a wider range of ASPECTS (2 to 5) to look for a potential threshold for EVT futility.
There is no going back. We showed the evidence, we showed the signal. These patients are more likely to benefit with thrombectomy. Amrou Sarraj
The trial ultimately included 300 patients (median age about 67; 53% men) randomized across 44 US sites to thrombectomy plus medical management or medical management alone. All had an intracranial ICA or MCA M1 occlusion with an NIHSS stroke of 6 or more (median roughly 19) and could be randomized within 24 hours of when they were last known to be well. One-fifth received IV thrombolytic therapy.
The primary efficacy endpoint was the 90-day utility-weighted modified Rankin Scale (mRS) score; the average was numerically better in the thrombectomy arm (2.93 vs 2.27), but the difference did not meet the threshold for superiority.
Some of the secondary outcomes pointed toward a benefit of EVT, however. The proportion of patients with an mRS score of 0 to 3 at 90 days was higher with thrombectomy (30% vs 20%; P = 0.03), as was the rate of major neurological improvement at day 5-7 (26% vs 13%; P = 0.0008). There was also a nonsignificantly greater improvement in quality of life according to the EQ-5D-5L score.
In terms of safety, there were no significant differences between the thrombectomy and control arms in 90-day mortality (35.3% vs 33.3%) or symptomatic ICH (3.97% vs 1.34%), although other hemorrhagic outcomes were increased with the intervention. Those included parenchymal hematoma type 1 (9.5% vs 2.7%) and type 2 (9.5% vs 3.4%), hemorrhagic infarction type 2 (21.6% vs 4.1%), and subarachnoid hemorrhage (16.2% vs 6.2%).
Pooled Results of the Three Prior Trials
Sarraj followed the presentation of those results with a pooled, patient-level meta-analysis of the RESCUE-Japan LIMIT, SELECT2, and ANGEL-ASPECT trials, conducted as part of an effort called the MAGNA Collaboration. Together, those trials included a total of 1,009 patients (median age about 69; 41% women) randomized to thrombectomy or medical management alone. The larger dataset improves estimates of the benefits of EVT in this setting, and allows for the assessment of important subgroups, Sarraj said.
The primary outcome of the pooled analysis was the distribution of mRS scores at 90 days, and not surprisingly considering the three trials were positive, this favored thrombectomy (adjusted generalized OR 1.78; 95% CI 1.48-2.14). When examined in dichotomized fashion, EVT was associated with higher rates of mRS 0-2 (23% vs 9%) and mRS 0-3 (41% vs 24%; P < 0.001 for both).
We’re chipping away at some of the tougher aspects of vascular neurology. Mitchell Elkind
There were no differences between the thrombectomy and control arms in mortality (27% vs 28%) and symptomatic ICH (1.8% vs 1.6%), but neurological worsening was higher in the EVT group (22% vs 17%; P = 0.01), “something that we explain by reperfusion and early cerebral edema,” Sarraj said. He added, “This did not detract from the treatment benefit, however.”
The procedural complication rate approached 10%, he reported, with dissection, perforation, and vasospasm each occurring in about 3% of patients.
Subgroup analyses mostly pointed toward a consistent benefit of thrombectomy, with better outcomes seen for patients with ischemic cores smaller than 150 mL (statistical significance was lost above that threshold). EVT was beneficial in patients with ASPECTS of 3, 4, or 5 assessed as individual categories. Results in the small group of patients with ASPECTS of 0-2 included in the trials were not definitive, Sarraj indicated.
The results “further emphasize thrombectomy efficacy and safety in this important population, potentially expanding the treatment to an additional 20%” of the population with acute strokes caused by large-vessel occlusions, he concluded.
Elkind said he was not ready to call for a change to guidelines based on the totality of the evidence around thrombectomy in large-core strokes, noting that none of the four trials have yet been peer-reviewed and published. But, he said, “I think we’ll start moving in that direction.”
Taking a step back, Elkind viewed the results in the context of other research presented at ESOC, including positive trials in patients with acute intracerebral hemorrhages.
“We’re chipping away at some of the tougher aspects of vascular neurology, and I think that’s exciting and tells us that we have a lot of room to go and neurological disease is certainly treatable,” he said. “That’s kind of a new era for us.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Yoo AJ, Zaidat OO. TESLA trial primary results. Presented at: ESOC 2023. May 26, 2023. Munich, Germany.
Sarraj A. Mechanical thrombectomy for large brain infarction (MAGNA collaboration). Presented at: ESOC 2023. May 26, 2023. Munich, Germany.
Disclosures
- TESLA was funded by unrestricted grants from Cerenovus, Penumbra, Medtronic, Stryker, and Genentech.
- Zaidat reports consulting for Stryker, Cerenovus, Penumbra, and Medtronic.
- Yoo reports consulting for Cerenovus, Penumbra, Vesalio, Rapid Medical, Zoll Circulation, Philips Neurovascular, and Nicolab.
- Sarraj reports serving as the global principal investigator for the SELECT2 trial, which was funded by research grants from Stryker Neurovascular.



Comments