Transcatheter Mitral, Tricuspid Valve Replacement Inch Forward
Promising results with the Intrepid TMVR and Evoque tricuspid systems set the stage for the pivotal trials now underway.
Early feasibility data from two studies of valve replacement presented at TCT 2021 show promise for novel transcatheter devices for mitral and tricuspid regurgitation.
The Intrepid (Medtronic) transcatheter mitral valve replacement (TMVR) early feasibility study showed no mortality, stroke, reintervention, or new pacemaker implantation within 30 days in the first 15 patients treated via the transseptal approach. Also, 6-month outcomes from the TRISCEND study confirmed what was seen at 30 days with significant reductions in tricuspid regurgitation (TR) and good survival following transcatheter implantation of the Evoque device (Edwards Lifesciences).
“This is the future,” commented Luigi Salemme, MD (Montevergine Clinic, Mercogliano, Italy), during a press conference. “We are moving to an interventional treatment of tricuspid and mitral disease.”
Intrepid EFS
 Firas Zahr, MD (Oregon Health and Science University, Portland), who presented the Intrepid findings, told TCTMD that “for an early feasibility study, these are very encouraging results.” The trileaflet bovine pericardial valve, which affixes to the mitral valve with outer stent anchors without capturing the native leaflets, is identical to that already being studied transapically in the ongoing APOLLO trial, where “the morbidity and mortality early on is very high due to the complications [related to] transapical access as well as its impact on the myocardial muscle,” Zahr said. With a transseptal delivery system, what is novel here, “the hope was that will address some of these concerns.”
Firas Zahr, MD (Oregon Health and Science University, Portland), who presented the Intrepid findings, told TCTMD that “for an early feasibility study, these are very encouraging results.” The trileaflet bovine pericardial valve, which affixes to the mitral valve with outer stent anchors without capturing the native leaflets, is identical to that already being studied transapically in the ongoing APOLLO trial, where “the morbidity and mortality early on is very high due to the complications [related to] transapical access as well as its impact on the myocardial muscle,” Zahr said. With a transseptal delivery system, what is novel here, “the hope was that will address some of these concerns.”
For the multicenter study, which was simultaneously published in JACC: Cardiovascular Interventions, Zahr and colleagues implanted 15 patients (mean age 80 years; 87% male) with at least moderate-to-severe symptomatic mitral regurgitation (MR) who were at high or extreme risk for mitral valve surgery with the Intrepid TMVR valve, which was mounted on a 35-Fr transfemoral delivery system. At baseline, 67% of patients were classified as NYHA class III or IV.
Average procedural time was 46 minutes, and most patients (93%) received the 48-mm valve. Notably, one patient was converted to a sternotomy due to valve migration. Atrial septal defect closure was performed in 73% of patients and mean length of stay was 5 days. One patient had a periprocedural MI due to an air embolism.
At 30 days, there were no reports of all-cause death, stroke, reintervention, new pacemakers, or acute kidney injury stage 2 or higher. Seven patients reported MVARC-defined major bleeding events, including six major vascular complications all related to the access site. One patient was rehospitalized due to a minor vascular complication.
Echocardiography at discharge showed 21% of patients with mild MR, but by 30 days all patients had none or trace MR. Paravalvular leak was seen in 7% at discharge but disappeared in all by 30 days. Also, LV outflow tract obstruction was moderate in 15% of patients at discharge, but zero or mild in all at 30 days.
Functional outcomes were good, with 57% and 29% being classified as NYHA class II and I, respectively, at 30 days.
Based on these results, Zahr reported that the transfemoral delivery system will now be rolled into the APOLLO pivotal trial. “Maneuvering the system has proven in the study to be relatively straightforward,” he said. “Despite the fact that it's early feasibility, most of the procedures were done under 1 hour because maneuvering the valve to the mitral annulus is very similar to maneuvering other devices that are commercially available in the mitral space.”
He admitted that the vascular complications observed were “a bit higher than we were hoping for,” although this is likely related to early experience and variability in anticoagulation regimens as well as “trying to figure out what's the best way to use the venous system for a large-bore sheath.” A 29-Fr delivery system is currently in development, Zahr said. “I'm hoping that as the sheath is getting smaller . . . as well as us learning what's the best way to manage vascular access and the best way for us to anticoagulate those patients perioperatively, that will hopefully address some of those bleeding complications.”
In the press conference, Rajiv Tayal, MD (Valley Health System, Ridgewood, NJ), said “this is clearly an exciting look into the future and very reassuring to a degree aside from the complications, which are somewhat expected as we go with 30-plus Fr devices. I think it's incredible and I'm very excited for it.”
Moderator Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), said she, too, was excited about the results even though “35-Fr scares the dickens out of me.” For the next phase, “this obviously would be best approached to see this in a smaller French size.”
TRISCEND at 6 Months
Presenting the 6-month results of TRISCEND, Susheel Kodali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said the Evoque system, which securely attaches into the tricuspid annulus by “engaging leaflets, chords, and the annulus,” demonstrated that the favorable 30-day outcomes were sustained at 6 months.
Of the 132 patients enrolled (mean age 79.2%; 74% female), 6-month follow-up was available for 56. Baseline TR grade was at least severe in 88% of patients and 90% had atrial fibrillation; 67% of patients were in class III/IV heart failure prior to implantation. Procedural device success was 96.2%, with most (94.7%) having right vein femoral access.
At 30 days, 18.5% reported major adverse events, including three cardiovascular deaths, one renal complication, 22 severe bleeds, two major access-site and vascular complications, two reinterventions, and one major cardiac structural complication. The all-cause mortality rate was 3.2% and eight patients required a new permanent pacemaker.
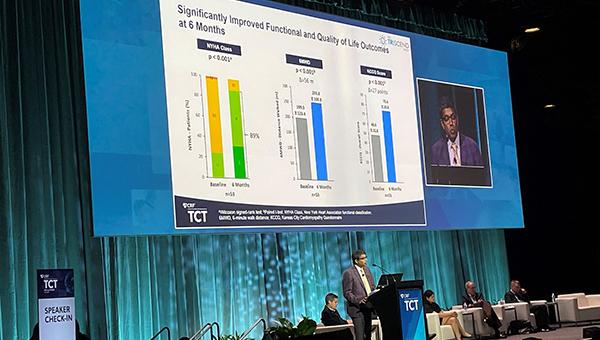
At 6 months, TR severity was mild in 49%, with the remaining 51% reporting none or trace levels (P < 0.001 vs baseline). Both the rates of survival (96%) and freedom from heart failure hospitalization (94%) were high at 6 months. Also, significant improvements were seen in NYHA class, with 89% of patients in class I or II at 6 months; 6-minute walk distance, with an increase of 56 m; and Kansas City Cardiomyopathy Questionnaire score, with an increase of 27 points (P < 0.001 for all).
As a result of these and earlier findings, the randomized pivotal TRISCEND II trial is already underway.
Kodali stressed to TCTMD the importance of new transcatheter devices to treat TR. “There's not really great options for these patients,” he said, adding that the number of patients he’s seen in the clinic over the last several years has been “steadily increasing.” Kodali also noted that challenges in this space have related to adequate imaging and that even the procedurally-challenging edge-to-edge technologies can still leave patients with moderate or even significant TR.
The biggest hurdle right now with this system relates to the high bleeding rate, he said. “A lot of them are not access-site—urinary tract, GI, other factors—but this is a patient population that has sort of high bleeding risk to begin with. But 17% at 30 days is definitely a significant bleeding rate and we need to understand why that is and we have to manage anticoagulation differently. It's important to dive more deeply into this and do better.”
Ultimately, the data show that “the device works,” Kodali said. “I think it's a reproducible procedure and I think from a feasibility standpoint it showed that it's feasible. You can eliminate TR, patients in general have done well. Whether this is clinically beneficial, I think the randomized trial is designed to show that.”
In the press conference, Mehran questioned the need for tricuspid replacement as opposed to repair. “It just seems like it's a big to-do,” she said. “Do you think that there are so many pitfalls to the repair that you need a replacement?”
Previous edge-to-edge repair studies like CLASP TR and TRILUMINATE have shown benefit but also have limitations related to “large gaps, broad jets, [and] imaging,” Kodali said. “So, there are trade-offs. I think over the next decade-plus we're going to need to understand which patients benefit which way and I think that's where the real knowledge gap is. We have a long way to go. We're just trying to get to the point [to know if] treating TR helps these patients.”
Tayal commented that this procedure “clearly seems to be a little bit more straightforward” than other investigational technologies to date.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Zahr F, Song HK, Chadderdon SM, et al. Thirty-day outcomes following transfemoral transseptal transcatheter mitral valve replacement: Intrepid TMVR early feasibility study results. J Am Coll Cardiol Intv. 2021;Epub ahead of print.
Kodali S. Tricuspid valve replacement in patients with tricuspid regurgitation: 6-month outcomes from the TRISCEND study. Presented at: TCT 2021. November 6, 2021. Orlando, FL.
Disclosures
- Zahr reports receiving institutional grant support from Edwards Lifesciences and Medtronic.
- Kodali reports receiving consultant fees from Admedus (now Anteris Technologies) and Dura Biotech; equity in Dura Biotech, Micro Interventional Devices, Thubrika Aortic Valve Inc, Supira, Admedus, TriFlo, and Anona; and institutional grant support from Edwards Lifesciences, Medtronic, Abbott Vascular, Boston Scientific, and JenaValve.
- Mehran reports grant support/research contracts (institutional) from Abbott Vascular, AstraZeneca, Bayer AG, Bristol-Myers Squibb, CSL Behring, Daiichi-Sankyo/Eli Lilly and Company, Medtronic, Novartis Pharmaceuticals, OrbusNeich, CERC, Chiesi, Concept Medical, Applied Therapeutics, Beth Israel Deaconess, Zoll, Arena, Biosensors, Boston Scientific, CellAegis, Insel Gruppe AG, Philips, and Transverse Medical; consultant fees/honoraria/speakers bureau fees (personal) from Medscape/WebMD, Janssen Scientific Affairs, Cine Med Research, ACC, CIRM, SCAI, and WebMD; equity < 1% (personal) from Elixir Medical, Applied Therapeutics, and STEL; equity < 1% to her spouse (personal) from ControlRad; advisory board payments (institutional) from Idorsia Pharmaceuticals; scientific advisory board payments (personal) from the AMA; consultant fees/honoraria/speakers bureau fees (institutional) from Abbott Vascular, Abiomed, AM-Pharma, Alleviant, Bayer, Beth Israel Deaconess, CardiaWave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; divested equity < 1% (institutional) from Claret Medical (now Boston Scientific); and scientific advisory board payments to her spouse (personal) from Biosensors.
- Salemme reports no relevant conflicts of interest.
- Tayal reports receiving consultant fees/honoraria/speakers bureau fees (personal) from Abiomed, Edwards Lifesciences, Abbott Vascular, and Shockwave Medical.




Comments