Use of IVC Filters for DVT Peaked in 2010 but Remains High
It took more than 10 years for physicians to respond to the absence of benefit in the PREPIC study, say researchers.
Despite clinical trial data showing inferior vena cava (IVC) filters are ineffective for reducing mortality following deep vein thrombosis (DVT), as well as guideline recommendations against their use in this setting, the proportion of patients with DVT given an IVC filter continued to rise over an extended period of time, according to the results of a new study.
The number of IVC filters inserted for patients with lone DVT peaked in 2009, however, and then declined over the following 5 years, report investigators.
Still, “both the number of IVC filters inserted yearly and the proportion of patients who received an IVC filter remained higher than in 1998 when a randomized controlled trial showed no reduced mortality with permanent IVC filters in patients with DVT,” write Paul Stein, MD (Michigan State University, East Lansing), and colleagues in their paper published online ahead of print August 22, 2019, in the American Journal of Cardiology.
Eric Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), who was not involved in the most-recent study, said their institution is much more conservative in 2019 than in the past when deciding on the use of IVC filters for patients with DVT. The falloff stems from the absence of a mortality benefit in the decades-old PREPIC trial, but also from concerns about potential complications with IVC implantation. Right now, the main indication for an IVC filter is thrombosis in a larger, proximal vein, such as the iliofemoral, and an absolute contraindication for anticoagulation.
“Usually, it’s when a patient with a new proximal DVT who has had a massive gastrointestinal bleed or subarachnoid hemorrhage, or some sort intracranial bleed, [and] can’t receive anticoagulation” that an IVC filter is considered, Secemsky told TCTMD. “Those are the ones where we’re considering a temporary filter until they can be back on anticoagulation. Similarly, when they also have concomitant [pulmonary embolism (PE)], which was excluded from this analysis, and you’re concerned about clot migration—that would be another reason [for an IVC filter]. Outside of that, when patients are already on therapeutic anticoagulation, we really don’t put in filters very commonly at all.”
PREPIC and Stubborn IVC Usage
The 400-patient PREPIC study showed that in patients with DVT at risk for PE, randomized to receive an IVC filter plus anticoagulation instead of anticoagulation alone, the filter significantly reduced the occurrence of PE at 12 days, but this was counterbalanced by an increase in the risk of DVT and lack of effect on mortality. Since then, clinical guidelines from the American College of Chest Physicians (ACCP) in 2008 and 2012, recommend the use of IVC filters only if there is a contraindication to anticoagulation.
To determine the response to the PREPIC study and the ACCP recommendations, researchers used administrative data from the National Hospital Discharge Survey (1979-2006) and Nationwide Inpatient Sample (2007-2014), identifying 8,523,098 patients between 1979 and 2014 with lone DVT. Among them, 705,162 received an IVC filter. The average age of patients treated with a filter was 70 years.
The number of IVC filters implanted in patients with lone DVT increased from 1979 to 2009, when use peaked at 51,288 implanted filters. In terms of the percentage of lone DVT patients receiving an IVC filter, the proportion also increased from 1979 but peaked in 2010, when 17.2% of all patients with lone DVT received a device. In 2014, the last year data were available from the Nationwide Inpatient Sample, 36,960 lone DVT patients received an IVC filter, or roughly 15% of all lone DVT cases.
“The reason for the continuing use of IVC filters in patients with lone DVT despite evidence and recommendations against their use in such patients is speculative,” write Stein and colleagues. “The present data suggest that at least 10 years passed before there was a noticeable effect of a randomized controlled trial showing negative results. This is concordant with the observation that may years may be required for the uptake of evidence into clinical practice.”
If a patient with DVT needs to stop anticoagulation therapy for a procedure and is not able to return to anticoagulant treatment for an extended amount of time, Secemsky said his hospital might temporarily place an IVC filter. He noted that one of the major differences between PREPIC and the current era is the development of removable IVC filters. “Now, when we put them in, we always create a timeline of when we want to have them out by,” he said.
The development of removable filters was an advance from permanent IVC filters studied in the 1990s, including in the PREPIC trial. This shift may have led to an increase in IVC filter use throughout in the 2000s, noted Secemsky. Even with PREPIC, the study showed the filters reduced the risk of PE, which some physicians may feel warrants their use in selective patients, he added. However, enthusiasm waned for their use following a 2010 US Food and Drug Administration safety communication warning about an increased risk of potential complications, such cardiac perforation, device fracture, and migration. As part of the safety communication, the FDA said the devices are no longer needed once there is no longer any concern about PE.
This warning, said Secemsky, also likely contributed to the declining use of IVC filters at the turn of this decade.
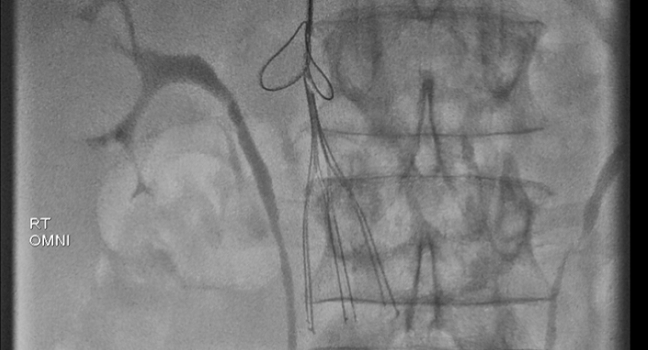
Photo Credit: Sista AK. Who should get an IVC Filter? Review of the guidelines. Presented at: TCT 2018. September 24, 2018. San Diego, CA.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Stein PD, Matta F, Hughes MJ. Continuing use of inferior vena cava filters despite data and recommendations against their use in patients with deep vein thrombosis. Am J Cardiol. 2019;Epub ahead of print.
Disclosures
- Stein and Secemsky report no relevant conflicts of interest.


Comments