Why I Chose a Career in Interventional Cardiology
Sometimes looking forward with ambition requires a look back with purpose.

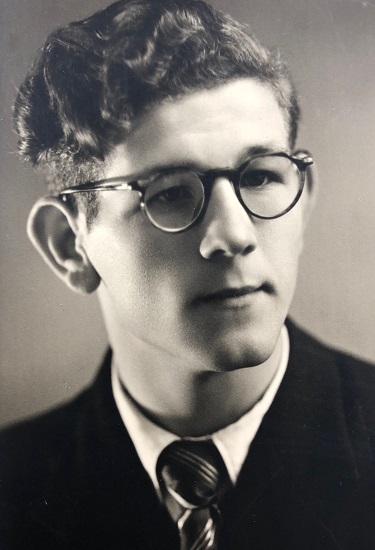
The reasons I went into medicine are multifactorial. First, I was inspired by family tradition. My grandfather was one of the first physicians to graduate in the then-new subspecialty of anesthesia. I have vivid memories of visiting him at his house Hasselt, Belgium after he had retired, and he would show me his portable anesthesia machine and tell me stories of how he would go around town from hospital to hospital to anesthetize patients. My father followed in his footsteps to become an anesthesiologist and intensivist, and he would show me pictures from when he was younger and part of the rapid response air brigade treating emergent patients in the coastal town of Bruges. Later on, they even worked together as colleagues for a few years in the same hospital.
The other reason is also family related. When people ask me if I have any siblings, I’ll say I have a sister and a brother. But really, I have a second brother who was born 2 years me before me, unfortunately with a condition called hypoplastic left heart syndrome. Today there are interventions available for patients like him, but at that time this condition was fatal within the first few days of life. Even though I never knew my brother, the stories told by my parents and the pain his death caused them certainly had an impact on my decision to go into medicine.
Attending medical school in Europe is very different from what it’s like in the United States. Students don’t go to college between high school and graduate training (eg, medical school, law school, business school), and the medical school programs are longer, usually around 6 years. It was while earning my medical degree at the Maastricht University in the Netherlands that my interest in cardiology was sparked.

I recall going into the basement of our medical school in the first few weeks of class of to attend gross anatomy sessions. We dissected each organ system slowly over the course of a trimester, and I clearly remember the session where we examined the complex anatomy of the various cardiac structures. As I progressed through my training, I continued to enjoy the topic of cardiology the most, whether this was practicing physical exam skills, sitting through lectures on cardiovascular physiology, or spending time in the coronary care unit. Yet, I was also fascinated by procedures and interventions during my surgery rotations. By the time I was nearing the end of my studies, I was sure I wanted to pursue a career studying and treating patients with cardiovascular disease, but I did not know if it would be best for me to become a cardiothoracic surgeon or an interventional cardiologist.
Around that same time, results from the first randomized clinical trial of TAVR—PARTNER Cohort B—were published. I still remember reading the article and being amazed that this treatment could reduce absolute mortality by 20% with a number needed to treat of five! At the time, my knowledge of this procedure and technology was very limited, though I understood that it would change the field of interventional cardiology. Patients with severe aortic stenosis up until that point had no other options, and suddenly, they had a treatment available that could prolong their life. I knew that not only would we be able to treat patients with coronary artery disease, but also we were opening the doors to treating valve disease percutaneously.

I pursued a postdoctoral fellowship at Duke University (Durham, NC) and internal medicine training at Northwestern University (Chicago, IL) and continued to follow the changes in the field of structural interventions. I observed with awe as TAVR grew mainstream and even newer technologies were being studied to treat mitral and tricuspid valve disease. Additionally, novel devices were emerging to prevent stroke in patients with A-fib. In the meantime, interventionalists were continuing to push the field of coronary interventions with more complex PCI, including left main and chronic total occlusions, and use percutaneous mechanical support devices.

It was this ongoing search and passion for innovation and rigorous clinical research among interventional cardiologists that really drove me to decide to become one myself. Looking forward, my main career goal is to push the field forward into the next decades of new frontiers.
A few weeks back I started a 2-year interventional cardiology fellowship that will involve not only rigorous procedural training in coronary, structural, and peripheral interventions, but also a significant research curriculum. This will most likely be one of the most important 2 years of my past decade of medical training, as it is the final transition into the role of an independent physician-scientist. As I start planning for a career in academic medicine, I hope I will always remember why I signed up for medicine in the first place and look ahead with a tremendous amount of energy and excitement to start contributing to the field of interventional cardiology.
018-2019 Fellow Talk Blogger
Lowie is an interventional cardiology fellow at Northwestern University (Chicago, IL), where he also trained in…
Read Full Bio

Comments