Worse Survival for Women After Ruptured AAA Repair
Women had higher perioperative and long-term mortality, and ruptured at smaller aneurysm diameters, SVS data show.

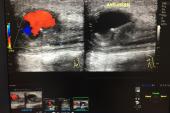
A nearly 20-year analysis sheds new light on sex disparities following abdominal aortic aneurysm (AAA) rupture and subsequent repair.
The study found that women were older than men, had aneurysms that ruptured at smaller diameters than the traditional threshold, and had worse in-hospital and long-term survival.
“Future studies would be useful to assess the reasons for these disparities and whether opportunities exist to improve AAA care for women, including more-frequent screening, better rupture-risk stratification, and strategies to reduce gender bias and discrimination,” write Ben Li, MD (Toronto General Hospital, Canada), and colleagues in the paper, published online May 10, 2022, in JAMA Network Open.
Overall, AAA is more prevalent in men than women and screening guidelines, while varied, primarily target older men. The US Preventive Services Task Force does not recommend that women undergo AAA screening. However, the Society for Vascular Surgery recommends a one-time screening for anyone aged 65 to 75 with a smoking history.
An expert who was not involved in the study agreed that the data deserve a “deep dive” to understand potential gaps in care that occur for women with AAA, or who are at risk for it, and how they can be addressed.
“We're still learning about the impact that sex differences have on aneurysm treatment, screening, and survival,” Grayson H. Wheatley, MD (Wheatley Surgical, Nashville, TN), told TCTMD. “This article certainly moves that analysis forward, but it also highlights that there's a lot more that we still have to learn.”
VQI Findings
For the study, Li and colleagues examined data on 1,160 women and 4,148 men from the Society for Vascular Surgery’s Vascular Quality Initiative (VQI) database who underwent AAA repair between 2003 and 2019. Compared with men, the female patients were older, more than twice as likely to be underweight, and more likely to be Black. Additionally, more women than men presented with chronic kidney disease (CKD) and chronic obstructive pulmonary disease. While the number of endovascular and surgical procedures was similar between women and men, there were physiologic differences seen in women, including smaller aortic neck diameters and aortic neck angle > 60 degrees.
In-hospital mortality was 34.4% in women and 26.6% in men (P = 0.002). The disproportionately higher death rate in women versus men remained in a subanalysis of patients aged 70 years or older (P = 0.008), and regardless of whether repair type was endovascular (P = 0.03) or open (P = 0.01). While in-hospital mortality decreased for both women and men over the course of the study, it remained higher for women at every individual time period.
Women’s 8-year survival rates were lower at 36.7% versus 49.5% for men (P = 0.02). Again, the difference persisted regardless of age or type of AAA repair. An additional analysis of differences in all-cause mortality rates beyond the perioperative period found that women continued to have lower survival at 8 years when only patients who survived beyond 30 days after the repair were included (P = 0.03).
In multivariable Cox regression analysis, older age, CKD, preoperative dialysis, congestive heart failure, previous carotid revascularization, unconscious at presentation, cardiac arrest, and open repair all were associated with 8-year all-cause mortality. The study authors say the latter finding deserves further research, since it is among the first to suggest a possible long-term mortality benefit of endovascular over open AAA repair.
Sex Bias and Ongoing Concerns
According to Li and colleagues, ruptured aneurysms were about 1 cm smaller in women than men. Along with the older age at presentation and prior studies documenting the underdiagnosis and undertreatment of AAA in women, they say these data suggest that “unconscious and conscious sex bias and discrimination prevalent in medicine and society may extend to AAA management.”
To TCTMD, Wheatley said accumulating data, including the finding of smaller size at rupture, point to a possible need to reevaluate screening recommendations for women, recognizing that these recommendations have traditionally been based on data from men.
“I think this presents a double opportunity not only to screen women earlier and more broadly, but to look seriously at the data to understand whether different treatment guidelines for elective aneurysm repair are warranted,” he said. “Women may have a different pathophysiology ,. . . and different screening and treatment guidelines therefore may apply.”
Wheatley cautioned that without looking at aorta-related mortality, however, it is hard to draw strong conclusions about the mortality differences or to rule out selection bias as a possible factor.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Li B, Eisenberg N, Witheford M, et al. Sex differences in outcomes following ruptured abdominal aortic aneurysm repair. JAMA Network Open. 2022;5:e2211336.
Disclosures
- Li reports no relevant conflicts of interest.



Comments