Ad Hoc PCI Safe and Feasible in Patients Undergoing TAVR
Same-session PCI for CAD plus TAVR resulted in a similar rate of composite death, disabling stroke, and MI as seen in patients undergoing TAVR alone.
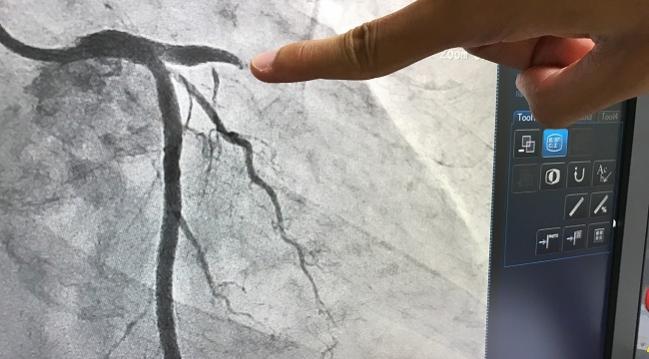
Screening for CAD using invasive coronary angiography as part of the patient work-up for transcatheter aortic valve replacement—and proceeding with PCI at the time of TAVR, if warranted—does not impact TAVR’s periprocedural risk or long-term outcomes, according to the results of a study published online August 2, 2017, in Circulation: Cardiovascular Interventions.
The findings offer important new insights, particularly as TAVR moves into younger, lower-risk patients, the authors say.
“This approach is controversial and we need to refine it, but in TAVR patients, it is feasible to screen for CAD and to perform ad hoc PCI in the same session,” Marco Barbanti, MD (University of Catania, Italy), told TCTMD. “The key issue will be to identify the TAVR population who would benefit most from this optimized approach.”
Barbanti and colleagues enrolled 604 consecutive patients deemed eligible for TAVR who then underwent CAD screening prior to their valve procedure. Severe CAD was treated with PCI; TAVR was then completed if the PCI was successful and uncomplicated, contrast dye was < 80 mL, and the patient was hemodynamically stable. The median age of patients was 82.
Severe CAD was identified in 136 patients (22.5%). Of these, 53 patients underwent an uncomplicated PCI procedure during the same session as their valve replacement. An additional 83 patients had severe CAD that was untreated for a variety of reasons including distal coronary stenosis or stenosis found in small vessels (49.4%), chronic total occlusions (31.3%), very high calcium burden (12.0%), or lesions subtending necrotic area (7.2%).
In two patients, TAVR was delayed by 1 month due to the large amount of contrast dye used during their PCI procedure.
For the cohort as a whole, 30-day all-cause mortality was 2.4% and the 30-day cardiovascular mortality was 1.4%. Rates of disabling stroke, MI, and life-threatening, major, and minor bleeding were also low, occurring in 0.5%, 0.8%, 4.0%, 17.9%, and 4.8% of patients, respectively. By 2 years, all-cause mortality was 12.9% and rates of disabling stroke and MI were 2.5% and 1.8%, respectively.
Importantly, authors saw no differences in key outcomes periprocedurally, at 30 days, or 2 years. At 2 years, the composite of death, disabling stroke, and myocardial infarction was roughly similar between those patients that underwent PCI plus TAVR (10.7%), patients found to have CAD that was left untreated (14.8%), and patients who underwent TAVR only (14.5%), with no significant differences between groups (log-rank P=0.855).
Same-Session Procedure
According to Barbanti, for many years, he and his colleagues have performed non-complex PCI procedures and TAVR in the same session. The reasons for this vary but include growing issues with long waiting lists for TAVR procedures.
“TAVR is now offered to many more patients, and it is foreseen that further expansion of the indication will happen very soon,” Barbanti said. “It is also becoming evident that local budget is not the only restriction for performing TAVR at many centers. Indeed, the number of TAVRs that can be performed is set by the availability of beds in the hospital.”
Commenting on the study for TCTMD, Josep Rodés-Cabau, MD (Laval University, Quebec City, Canada), observed that the demand for TAVR is very variable by center and country, but that the number of TAVR procedures performed is definitely increasing.
Rodés-Cabau, who wrote an editorial accompanying the study, said that the new results speak to the safety and feasibility of combining coronary angiography/PCI and TAVR but with the caveat that only one in four patients in this study had complex CAD. Previous studies, as Rodés-Cabau noted in his editorial, have included patients with rates of severe CAD of 50% or more.
Barbanti agreed that not all patients can benefit from this approach, adding that it will be important to identify a subset in whom this strategy can guarantee the highest level of safety and cost-effectiveness.
For example, Rodés-Cabau noted, the higher amount of contrast may increase the risk of contrast nephropathy, particularly in those patients with moderate-to-severe chronic kidney disease.
“In intermediate-to-high risk—but operable—patients, the presence and severity of coronary artery disease may be an important factor in the clinical decision-making process for TAVR versus SAVR,” he said. “These decisions may be more difficult when the patient is already scheduled for a TAVR procedure immediately after coronary angiography.”
Obtaining the good outcomes seen with this approach will be dependent on clinicians discussing each case with the heart team and setting reasonable thresholds for PCI in the presence of severe CAD, Barbanti said.
Sources
Barbanti M, Todaro D, Costa G, et al. Optimized screening of coronary artery disease with invasive coronary angiography and ad hoc percutaneous coronary intervention during transcatheter aortic valve replacement. Circ Cardiovasc Interv. 2017;Epub ahead of print.
Rodés-Cabau J. Combining transcatheter aortic valve replacement and coronary angiography/percutaneous coronary intervention procedures: ready for prime time? Circ Cardiovasc Interv. 2017;Epub ahead of print.
Disclosures
- Barbanti reports serving as a consultant for Edwards Lifesciences.
- Rodés-Cabau reports receiving research grants from Edwards Lifesciences and Medtronic.
Comments