Antiplatelets, Especially Cilostazol, Helpful in Moyamoya Arteriopathy
New observational data hint that antiplatelets may cut deaths in this rare cerebrovascular disorder, but RCTs are urgently needed.

New data from an observational study provide some support for antiplatelet therapy in patients with moyamoya disease, a rare arteriopathy characterized by progressive stenosis of the distal internal carotid artery and other basal cerebral arteries.
Patients with moyamoya disease prescribed antiplatelet therapy, tracked through the Korean National Health Insurance Service (NHIS) database, had a significantly lower risk of death than those who didn’t receive antiplatelet therapy (HR 0.77; 95% CI 0.70-0.84). The largest reduction in mortality was seen in patients who were prescribed the phosphodiesterase inhibitor cilostazol (HR 0.57; 95% CI 0.49-0.68).
Based on their findings, “antiplatelet therapy generally, and cilostazol particularly, shows observational evidence of potential benefit as medical treatment for patients with moyamoya disease,” write Woo-Keun Seo, MD, PhD (Samsung Medical Center, Seoul, South Korea), and colleagues in their study published February 22, 2021, in the Journal of the American Heart Association. “These findings merit validation by testing in formal randomized clinical trials.”
Study author Jeffrey Saver, MD (University of California, Los Angeles), said the leading treatment for moyamoya disease is surgery with either direct or indirect revascularization to increase cerebral blood flow. Medical therapy is used in patients with mild disease or as an adjunct to surgery, but the evidence base supporting such use is weak, he told TCTMD, which is the reason they performed the analysis.
“The chief [medical] strategies are antiplatelet therapy, often with aspirin, and combined antiplatelet and cerebral vasodilatory therapy with cilostazol,” said Saver. “Antiplatelet agents may help reduce thrombosis occurring in slow-flow vessels. But moyamoya patients are also prone to intracerebral hemorrhage as their small deep arteries are overloaded and prone to rupture, so use of these agents is not risk free.”
However, there has been a growing sense that hemorrhage is relatively rare in patients with mild moyamoya disease who don’t require surgical revascularization and in patients who have had a successful response to surgery. “Accordingly, [antiplatelet] use has been increasing, especially cilostazol,” said Saver.
Edward Smith, MD (Children’s Hospital Boston, MA), a pediatric cerebrovascular surgeon who’s a leading expert in the treatment of moyamoya disease, said the present study provides compelling evidence about antiplatelet therapy’s benefits. “This suggests that the combination of the current standard of treatment, surgical revascularization, now has evidence from research with a large national cohort in Korea of more than 9,000 patients, that supports use of a specific medical therapy to improve outcomes,” he told TCTMD in an email.
Cilostazol’s Benefit in Multiple Subgroups
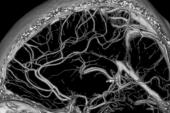
Moyamoya, in Japanese, translates roughly as “puff of smoke” and is used to describe the appearance of tiny collateral vessels on imaging that result from stenosis of the intracranial arteries. The cause of moyamoya disease is unknown, but it is believed it may have genetic determinants. Incidence is highest in East Asian countries, particularly Japan, Korea, and China, but the disease does affect people around the world. While moyamoya can occur at any age, symptoms typically occur in children between age 5 and 10 and in adults in their 30s and 40s, with stroke or recurrent transient ischemic attack the first sign that anything is amiss. Other symptoms include headache, seizures, visual disturbances, weakness/paralysis, and involuntary movements.
At present, cerebral revascularization surgery is selectively performed in patients with ischemic symptoms. Japanese guidelines recommend the oral administration of antiplatelet agents to prevent ischemic events, but they acknowledge there is little evidence to support that recommendation. The US Food and Drug Administration has yet not approved antiplatelet or anticoagulant therapies for patients with moyamoya disease.
In the Korean NHIS, the researchers identified 25,978 patients with newly diagnosed moyamoya disease, mean age 37.6 years, who were followed for an average of 6.3 years. At the time of diagnosis, more than one-third had already had an ischemic stroke, 20.4% a hemorrhagic stroke, and 50% any type of stroke. In total, 9,154 of patients were prescribed antiplatelet therapy at least once during the follow-up period, most commonly aspirin (55.2%) followed by clopidogrel (38.0%), others (8.1%), and cilostazol (5.5%). Use of cilostazol increased rapidly after 2003, however, and by 2013 was the most prescribed antiplatelet agent. In 2016, 52.4% of all patients received cilostazol.
In terms of the treatment benefit, cilostazol was the only antiplatelet agent that reduced mortality in patients younger than 45 years, 45 years and older, in those with a history of ischemic stroke, and those with a history of hemorrhagic stroke.
The current study, say investigators, “supports differential efficacy and safety of cilostazol as an antiplatelet agent in patients with moyamoya disease.” Mechanistically, phosphodiesterase inhibitors, like cilostazol, possess additional features not shared by other antiplatelet agent classes, including vasodilatory effects, which can improve collateral blood flow. For Saver, the clinical message from their observational study is that physicians can consider antiplatelet agents, especially phosphodiesterase inhibitors like cilostazol, to prevent ischemic stroke but still should “be aware that the evidence currently is only suggestive and randomized trials are needed.”
The researchers acknowledge the limitations of their analysis, notably that antiplatelet therapy use in the NHIS was the result of physician discretion rather than randomization. While propensity-score matching and time-dependent survival analyses eliminate some of the potential for bias, residual or unmeasured confounding could still be present, they write. Saver highlighted the potential for healthy cohort bias, whereby healthier patients are treated more aggressively. “Randomized controlled trials are needed to provide a truly unbiased assessment,” he said.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Seo W-K, Kim J-Y, Choi E-H, et al. Association of antiplatelet therapy, including cilostazol, with improved survival in patients with moyamoya disease in a nationwide study. J Am Heart Assoc. 2021;10:e017701.
Disclosures
- Seo reports receiving honoraria for lecture from Pfizer, Sanofi-Aventis, Dong-A Pharmaceutical Co., Beyer, Daewong Pharmaceutical Co., Daiichi Sankyo, and Boryung Pharmaceutical. He reports a study grant from Daiichi Sankyo and consulting fees from JLK Inspection.
- Saver reports payments from Boehringer Ingelheim for serving on a clinical trial steering committee.




Comments