Antithrombotics Not Worth the Risk During Endovascular Stroke Therapy
Aspirin and/or heparin doubled symptomatic ICH, without improving functional outcomes, in the MR CLEAN-MED trial.

Giving IV aspirin and/or unfractionated heparin during endovascular stroke treatment does not seem to be a good idea, at least at the doses evaluated in the MR CLEAN-MED trial.
In the study, such treatment failed to improve functional outcomes and doubled the risk of symptomatic intracranial hemorrhage (ICH) among patients with acute ischemic stroke, according to researchers led by Wouter van der Steen, MD (Erasmus MC University Medical Center, Rotterdam, the Netherlands).
The idea had been that providing antithrombotic therapy, on top of clot removal, would address lingering incomplete reperfusion of smaller vessels behind the main blockage and further improve the results of a procedure that has already been shown to provide substantial benefits in patients with large-vessel occlusions. Some operators are already doing this—with observational data suggesting a positive impact despite a modest increase in symptomatic ICH—but MR CLEAN-MED is the first randomized trial to put the approach to the test.
The results, published online last week in the Lancet, show that “if there were beneficial effects, they didn’t outweigh the added risk of symptomatic intracranial hemorrhage,” van der Steen told TCTMD.
“We advise not to use the evaluated dosages of unfractionated heparin and acetylsalicylic acid during endovascular stroke treatment,” he said. He pointed both to the increase in bleeding and to the nonsignificant trends toward worse functional outcomes, which, he said, might have been significant had the trial not been stopped early due to safety concerns.
MR CLEAN-MED
The trial, conducted at 15 Dutch centers, enrolled 663 adults (median age 73 years; 47% women) who had an ischemic stroke due to an intracranial large-vessel occlusion in the anterior circulation; had an NIHSS score of 2 or more (median 15); had brain imaging that ruled out an ICH; and underwent endovascular therapy within 6 hours of symptom onset or the time they were last seen well. The planned enrollment was 1,500, but MR CLEAN-MED was halted when interim analyses revealed increases in symptomatic ICH in the antithrombotic groups.
The patients were randomized 1:1 to periprocedural IV aspirin (300 mg bolus) or no aspirin and also 1:1:1 to moderate-dose unfractionated heparin (5,000 IU bolus followed by 1,250 IU/h for 6 hours), low-dose unfractionated heparin (5,000 IU bolus followed by 500 IU/hour for 6 hours), or no heparin. The median time to bolus administration was 5 minutes for aspirin and 6 for heparin.
Endovascular therapy involved thrombectomy in 86% of cases, digital subtraction angiography in 9%, and catheterization alone in 2%; ultimately, 3% did not have an endovascular procedure performed. In addition, 5% of patients underwent acute carotid stenting and 7% percutaneous transluminal angioplasty.
The primary outcome of the trial was the modified Rankin Scale score at 90 days, with nonsignificant trends toward worse function in patients who received aspirin (adjusted common OR 0.91; 95% CI 0.69-1.21) or unfractionated heparin (adjusted common OR 0.81; 95% CI 0.61-1.08). For heparin, the negative trend was driven by those who received moderate versus low doses.
Although use of unfractionated heparin was associated with an increased likelihood of complete recanalization at 24 hours (OR 1.89; 95% CI 1.16-3.09), there were no differences observed for any other secondary outcomes.
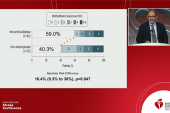
And that was not enough to overcome the damage from symptomatic ICH, which was twice as common in patients who received aspirin (14% vs 7%; adjusted OR 1.95; 95% CI 1.13-3.35) or unfractionated heparin (13% vs 7%; adjusted OR 1.98; 95% CI 1.14-3.46) compared with those who didn’t receive additional antithrombotic therapy. All-cause mortality was numerically, but not significantly, more frequent with either aspirin or heparin; moderate doses of heparin were associated with greater risk.
Van der Steen said the doses of aspirin and heparin evaluated in MR CLEAN-MED are already used in practice. Lower doses are used, as well, and it’s unclear how those would perform in a randomized trial. “We cannot make definite statements on the use of lower dosages,” van der Steen acknowledged. “However, with the results of our trial, we consider it wise to evaluate them before they remain or become usual practice.”
Additional Trials Needed
Commenting for TCTMD, Fadi Nahab, MD (Emory Healthcare, Atlanta, GA), said that even though he was excited to see a randomized trial addressing the use antithrombotic therapy during stroke thrombectomy, the results “highlight that additional trials are needed to better clarify what the optimal treatment will be.”
He said he was “taken aback” by the bolus doses of heparin used in the trial, noting that prior observational studies by his group suggested benefits of using lower median doses of 2,000 to 3,000 IU. “So it’s very much possible that a lower heparin dose may actually provide a better risk-benefit profile in patients treated with thrombectomy,” Nahab said. Even in MR CLEAN-MED, he noted, there was some signal of benefit with heparin, which increased recanalization at 24 hours.
Moreover, he pointed out that roughly three-quarters of patients in the trial received IV tissue plasminogen activator (tPA) before thrombectomy. That’s a key detail because the ARTIS trial—conducted before thrombectomy was established as standard of care—showed that using IV aspirin in patients treated with IV thrombolysis increases the risk of symptomatic ICH.
“The expectation that intracranial hemorrhage rates are not affected by whether a patient receives IV tPA or not is unrealistic,” Nahab said, adding that one should be “very cautious” about giving aspirin after IV tPA in patients undergoing thrombectomy. “The optimal antithrombotic regimen is likely to be different in patients who receive IV tPA versus those who don’t.”
And one final limitation of the trial, Nahab indicated, is that the investigators didn’t taken into account whether patients were already on antithrombotic therapy at the time of their stroke. These medications can last in a patient’s system for days, so it will be important for future trials to take that into consideration, he said.
Mohammed Almekhlafi, MD, and Shelagh Coutts, MD (both University of Calgary, Canada), highlight some of the same issues in an accompanying editorial, and say “the effects of these results on current practice and future research are hard to predict.”
As for whether there’s a place for anticoagulation or antiplatelet therapy in acute stroke, “the answer is possibly not among those receiving thrombolytic therapy before thrombectomy,” Almekhlafi and Coutts write. “How about those who are not candidates for intravenous thrombolysis? Does the expected benefit of microvascular reperfusion outweigh the risks of hemorrhage? These questions have not been fully answered by this trial; however, other trials are ongoing.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Van der Steen W, van de Graaf RA, Chalos V, et al. Safety and efficacy of aspirin, unfractionated heparin, both, or neither during endovascular stroke treatment (MR CLEAN-MED): an open-label, multicentre, randomised controlled trial. Lancet. 2022;Epub ahead of print.
Almekhlafi MA, Coutts SB. Anti-thrombotics cause harm in the setting of stroke thrombectomy. Lancet. 2022;Epub ahead of print.
Disclosures
- The study was funded by the Collaboration for New Treatments of Acute Stroke (CONTRAST) consortium, which acknowledges support from the Netherlands Cardiovascular Research Initiative, an initiative of the Dutch Heart Foundation; the Brain Foundation Netherlands; the Ministry of Economic Affairs, by means of the public–private partnerships allowance made available by Top Sector Life Sciences & Health to stimulate public–private partnerships; and in part through unrestricted funding by Stryker, Medtronic, and Cerenovus.
- Van der Steen, Nahab, Almekhlafi, and Coutts report no relevant conflicts of interest.




Comments