Better Closure, More A-fib With Cardioform for PFO Closure: Retrospective Series
Operators generally have their device preferences, but an expert states that though A-fib is transient, effective closure is forever.
A retrospective comparison of six patent foramen ovale (PFO) closure devices used in the United States over 18 years shows a trade-off between effectiveness and arrhythmia. Specifically, the Cardioform septal occluder (WL Gore) resulted in successful closure in every procedure in which it was used, but 13% of patients developed transient A-fib.
“This study demonstrates that, among six different PFO occluders used across 320 subjects, the Cardioform device achieved the highest effective closure rate but at the expense of a higher frequency of atrial fibrillation,” write lead author Rubine Gevorgyan Fleming, MD (University of California, Los Angeles), and colleagues. “These two observations are presumably related by the stronger force between the two disks used in this device compared with the previous Helex model. The stronger attractive force provides more effective closure but may produce more irritation.”
Commenting on the study for TCTMD, Robert Sommer, MD (NewYork-Presbyterian Hospital/Columbia University Irving Medical Center, New York, NY), said he was surprised by the findings given that “everybody always claims that the Amplatzer devices have the best closure rates.”
What PFO operators can take away from this experience is “that, for whatever reason, the Cardioform seems to cause a more vigorous reaction from the myocardium of the septum and that's what's causing the arrhythmias, but it's also probably what's closing the holes,” he said. “In all these patients, the atrial fibrillation is transient but the closure is forever.”
Moreover, A-fib is a known complication of PFO closure, one that physicians already discuss with their patients, Sommer added. “As far as we know, even with the risk of atrial fibrillation by putting in a device, all of the trials still showed that you were safer from having a stroke than if you left the hole open. So that's easy.”
The findings were published online October 26, 2019, ahead of print in Catheterization and Cardiovascular Interventions.
Six Devices, Various Outcomes
For the study, Fleming and colleagues retrospectively looked at 320 patients who received PFO closure as well as quantitative assessment of right-to-left shunting before and after their procedures, which occurred at UCLA between February 2001 and July 2019. The following devices were investigated:
- Amplatzer ASO (n = 17)
- Amplatzer PFO (n = 33)
- Amplatzer Cribriform (n = 14)
- WL Gore Helex (n = 132)
- WL Gore Cardioform (n = 105)
- NMT CardioSEAL (n = 14)
Patients who received the Amplatzer ASO device had a wider PFO canal than others because this occluder was originally chosen to treat larger PFOs. The PFO length was largely consistent among all the devices, with the exception of the Cardioform, which had a greater mean length.
Effective closure rates were greatest for the Cardioform and Cribriform devices, and the shortest times from device placement to effective closure were seen in the Cardioform group.
PFO Closure Outcomes
|
|
Mean Effective Closure Time, months |
Effective Closure Rate |
|
Cardioform |
2.3 |
100% |
|
Amplatzer Cribriform |
12.7 |
93% |
|
Helex |
5.7 |
90% |
|
Amplatzer ASO |
3 |
88% |
|
CardioSEAL |
– |
86% |
|
Amplatzer PFO |
– |
85% |
|
P Value |
< 0.001 |
0.004a 0.007b |
aCardioform vs Helex. bCardioform vs Amplatzer PFO.
Mild chest pain was reported by patients in each of the device groups (average 13.3%). One patient in the Cardioform group needed prompt surgical extraction of the device due to a wire frame fracture causing cardiac tamponade. One patient who received Helex had device embolization requiring endovascular removal and percutaneous placement of a new device. Lastly, three patients from the CardioSEAL cohort reported thrombus formation on the device.
In a subgroup analysis, patients who received the Helex device had a lower incidence of A-fib than those who received the Cardioform (4% vs 13%; P < 0.01). For comparison’s sake, data from the RESPECT trial show a 4% A-fib rate with Amplatzer PFO and data from the REDUCE trial show 5% and 7% A-fib rates associated with the Helex and Cardioform devices, respectively.
“Although the Cardioform device yields a lower residual shunt rate, it places patients at a higher risk of developing transient atrial fibrillation, thereby emphasizing the need to balance risks and benefits when choosing which device to use when closing a PFO,” the authors write. “All of the clinical trials that looked at PFO closure as a means of preventing recurrent cryptogenic stroke, as well as this study, likely underestimate the true incidence of atrial fibrillation because consistent ECG monitoring was not performed following the procedure. ECG monitoring with an implantable monitor is superior to conventional follow-up for detecting this arrhythmia after cryptogenic stroke.”
Prospective A-fib Data Needed
Notably, the Cardioform device “is the most contemporary of all the devices used, so there may be some selection bias in that techniques are improved and understanding of the procedure is improved,” Sommer said. “It's not a contemporary randomized trial, so there definitely are some issues with the methods, but nonetheless the results were interesting.”
With regard to A-fib, other trials have shown a higher rate associated with the Cardioform device, “but it was never really this high—13% is about twice what we saw in the randomized prospective trial,” he noted. “Of course this is all retrospective, but I believe . . . that Amplatzer seems to have the least arrhythmogenicity of all of the devices.”
Sommer said he prefers using the Cardioform device, acknowledging that while sometimes patient anatomy calls for one occluder over another, most physicians stick with their preferred choice. “The Amplatzer device is almost idiotproof—it's ridiculously simple to use,” he said. “If you don't like how it went in, you can collapse it and reuse it. The Helex, the Cardioform, the Cardioseal, those were all much, much more complicated to retrieve, and so ultimately what turned out was that people who had a low volume were all using Amplatzer and people who had bigger volumes were using some of the other devices, and I think it's kind of really stayed along those lines.”
Going forward, “we now need prospective trials which will assess the clinical incidence, relevance, and time course of the atrial fibrillation after PFO closure,” he concluded.
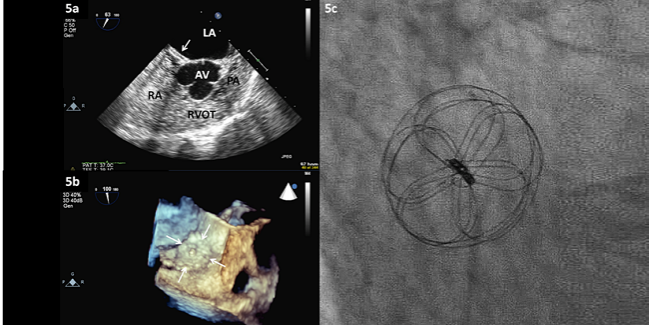
Photo Credit: Sondergaard L. PFO closure with the CardioForm: device description, ideal and non-ideal anatomy, technique, and complications. Presented at: TCT 2018. September 22, 2018. San Diego, CA.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Fleming RG, Kumar P, West B, et al. Comparison of residual shunt rate and complications across 6 different closure devices for patent foramen ovale. Catheter Cardiovasc Interv. 2019;Epub ahead of print.
Disclosures
- The paper provides no conflict of interest statement for Fleming.
- Sommer reports serving as the national co-PI on the ASSURED trial sponsored by Gore and also as the national cardiology PI for an upcoming migraine PFO trial sponsored by Gore.


Comments