For Bifurcation Lesions, It’s OK to Start With Just One Stent: EBC Trials
At 3 years in EBC MAIN and 5 years in EBC TWO, the provisional strategy did just as well as—or better than—dual stenting.

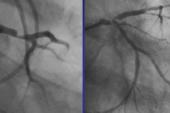
PARIS, France—A stepwise, provisional approach to PCI in bifurcation lesions continues to offer similar outcomes compared with a strategy in which two stents are the plan from the outset. Here at EuroPCR 2023, researchers from the European Bifurcation Club (EBC) released new follow-up data from two trials backing the idea that it’s okay to start with a single stent.
At 3 years, EBC MAIN—as it did in previously released 1-year results—showed no differences in the primary composite of death, MI, and revascularization between the two tactics for left main (LM) bifurcations. But this time around, TLR rates favored the stepwise, provisional arm.
And in non-LM bifurcations, 5-year findings from EBC TWO showed no advantage for routine culotte over provisional stenting. The data were simultaneously published online in EuroIntervention.
David Hildick-Smith, MD (Brighton and Sussex University Hospitals, Brighton, England), presenting the EBC MAIN results, stressed that there’s a straightforward message: “It is not necessary to decide before you do the case how many stents you’re going to put in.”
Philip Urban, MD (L'Hôpital de la Tour, Geneva, Switzerland), a discussant in the late-breaking EuroPCR session featuring EBC MAIN and EBC TWO, said that the two trials fit perfectly together. “I think the picture is getting clearer and clearer: you try and stay away from that second stent,” he affirmed.
Also presented in this session was the KISS trial, which looked at whether it’s possible to skip the side branch entirely under certain conditions: when the main-branch stent is sized to the distal reference diameter with a systematic proximal optimization technique (POT) and the side branch is patent with no flow reduction or signs of ongoing ischemia. Compared with side-branch intervention (kissing balloon or POT/side/POT), the simpler strategy came out ahead at 30 days.
Moderator Davide Capodanno, MD, PhD (University of Catania, Italy), speaking with TCTMD, said that the bifurcation trials “reinforced my practice. Because having long-term data, it’s reassuring that what we’re doing is okay.”
KISS, meanwhile, is unique in that it enables operators to not worry about addressing the side branch after a successful main-branch intervention. The study “somehow makes me feel less guilty when I say, ‘Okay, it’s over. I don’t want to treat that side branch.’ That’s new. Because sometimes you feel [like you] have to strive for the best possible outcome, but in the end, probably, it’s more harmful than beneficial,” Capodanno said. “This is something new I discovered.”
EBC MAIN in the LM
EBC MAIN randomized 467 patients from 11 European countries to either a stepwise, provisional strategy or systematic dual-stent approach (Resolute Onyx; Medtronic) to LM bifurcations. The choice of technique (culotte, DK-minicrush, T/TAP) was left to the discretion of the operator, but proximal optimization and kissing balloon technique were mandated in both groups. In the provisional group, 22% ultimately received a second stent.
It is not necessary to decide before you do the case how many stents you’re going to put in. David Hildick-Smith
At 3 years, the combined rate of death, MI, and revascularization was similar for provisional versus systematic dual stenting (23% vs 29%; P = 0.13). Also similar were death (10% vs 13%; P = 0.27) and MI (12% vs 11%; P = 0.75). Yet the TLR rate was significantly lower with the provisional strategy (8% vs 14%; P = 0.02); irrespective of which approach was used, most of these repeat interventions occurred in the ostium of the circumflex.
“I think firstly it’s important to say, looking at the outcomes overall, the results are good—these are patients with bifurcation left main stem disease. It’s a pretty ugly situation for people, but the outcomes were actually pretty good with stenting for both groups,” Hildick-Smith said.
And in the provisional group, in addition to having less TLR, nearly four in five patients avoided a second stent, he emphasized. This resulted in shorter procedure time, lower X-ray dose, and fewer resources used with the stepwise strategy.
Capodanno, after Hildick-Smith’s presentation, described the latest EBC MAIN report as a “very interesting follow-up extension.”
And indeed it holds some surprises, he said, “because we are starting to see some divergence in the curve over time—and I must say, personally, not in the direction I would have expected. No, I would have expected that two stents maybe in the future will be protective somehow. But actually it’s harmful, apparently, in terms of TLR.”
Capodanno asked if these interventions are ischemia-driven TLR or perhaps “that group had more angiographic follow-up, because the physician was concerned that there were two stents and they wanted to check.”
There was no routine angiographic follow-up as part of EBC MAIN, Hildick-Smith said. “So this is a very pragmatic, clinically based study. Everyone was free to follow-up patients as they saw fit and do angiography on the basis of whatever ischemic tests they had organized.” Capodanno agreed that the progressive divergence of the curves over time likely “suggests that there are new events and new ischemia” occurring.
Urban, based on what Capodanno observed regarding potential harm, said a burning question now is how a drug-eluting balloon would do in the side branch.
“I think what’s really interesting about that is that increasingly, maybe over the last 2 years or so, at least in my brain anyway, it’s become apparent that a stent isn’t ‘for free,’” Hildick-Smith observed. “Once you’ve put a stent in, you’ve left something which is a source of permanent, persistent—is it inflammation, what is it exactly? But [regardless], it’s a nidus for something else to happen. And therefore I’m not surprised that we’ve found two stents is less good than one stent. And probably no stent is better than one stent, if you’re able to get there and do it.”
He predicted that there is “going to be a sea change where we look to avoid the implantation of permanent metalwork. Over the course of the next 5 years, we’re going to learn a lot, again, about how to do that.”
EBC TWO in Non-LM Lesions
Sandeep Arunothayaraj, MBBS (University Hospitals Sussex NHS Foundation Trust, Brighton, England), opened his presentation of the EBC TWO findings reminding EuroPCR attendees that earlier randomized trials, like the Nordic Bifurcation Study and BBC ONE, found neutral or worse results for two stents. This may have been due to the use of first-generation devices or the stenting of small, possibly not functionally significant side branches, he suggested.
EBC TWO randomized 200 European patients with non-LM bifurcations to provisional versus culotte stenting with a Nobori device (Terumo Corporation). All had a side-branch diameter ≥ 2.5 mm and side-branch lesion length > 5 mm. Only 16% of the patients randomly assigned to the provisional cohort wound up having side-branch stents.
I think the picture is getting clearer and clearer: you try and stay away from that second stent. Philip Urban
At 1-year follow-up, the primary endpoint of MACE was similar for the provisional and systematic culotte groups (7.7% vs 10.3%; P = 0.53). In the newly released 5-year follow-up, this similarity was maintained (18.4% vs 23.7%; P = 0.36), with no differences for all-cause death, MI, or TVR individually. Nor was there an interaction based on whether side-branch lesion length was above or below the cut point of 10 mm.
Bifurcation-related adverse cardiac events (acute vessel closure, probable or definite stent thrombosis, type 1 MI, or revascularization) were rare and equally distributed between the two groups (5.8% vs 7.2%; P = 0.69).
“I think, reassuringly, this suggests we can achieve excellent long-term outcomes . . . using both modern stents and modern PCI techniques. It’s also then apparent that the majority of the outcomes in the MACE overall finding were from de novo lesions, and this illustrates really the importance of excellent secondary risk factor control for these patients,” Arunothayaraj said.
He concluded: “The provisional strategy should continue to be the default approach for true bifurcation disease.”
Urban agreed that “having long-term follow-up of this degree is extremely important.”
“Your data supports the fact that you should use one stent if you can, and two only if you must,” he said. Unanswered is whether there might be certain subgroups likely to benefit from an up-front two-stent approach.
In reply, Arunothayaraj said that the vast majority of bifurcation lesions seen in real-world clinical practice would do well with the provisional strategy. Even when the side-branch disease is lengthy, good results can be achieved through balloon alone rather than a second stent, he added. However, “I think there are situations that can come to mind where, for example, if you have a side branch and main vessel dissection and you do not want to lose access to that vessel, you do not want to rewire that vessel, you may then change your technique to an upfront two-stent technique. But that would definitely be the less-common situation.”
One caveat, said Arunothayaraj, is that these long-term results reflect the practice patterns of 2011 to 2014; changes to stent platforms, vessel preparation, and medical therapy might all influence results.
“All these factors together may mean that actually the bifurcation [results] we get from here on in, the adverse events rates, are even lower than what they were with this trial. . . . But I think overall this shows that we are on the right track and that we do achieve good outcomes,” Arunothayaraj concluded.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Hildick-Smith D. The European Bifurcation Club Left Main Coronary Stent study - a randomised comparison of stepwise provisional versus systematic dual stenting strategies (EBC MAIN): 3 year results. Presented at: EuroPCR 2023. May 16, 2023. Paris, France.
Arunothayaraj S, Behan MW, Lefèvre T, et al. Stepwise provisional versus systematic culotte for stenting of true coronary bifurcation lesions: five-year follow-up of the multicentre randomised EBC TWO Trial. EuroIntervention. 2023;Epub ahead of print.
Disclosures
- Hildick-Smith reports serving as a proctor/advisor to Boston Scientific, Abbott, Medtronic, Edwards, and Terumo.
- EBC MAIN was supported by an educational grant from Medtronic.
- Arunothayaraj reports no relevant conflicts of interest.
- EBC Two was funded by an unrestricted grant from Terumo Europe, with additional funding for core lab analysis from Pie Medical Imaging.




Comments