CUTTING-EDGE Insights into MV Surgery Outcomes After Failed Clip Procedures
The registry, with 15 years’ worth of data, indicates that mortality after do-overs “is not trivial,” Gilbert Tang reports.
First results from the long-running CUTTING-EDGE registry provide insights into the reasons for mitral valve surgery following transcatheter edge-to-edge repair (TEER), the types of surgeries performed, and how patients fare thereafter.
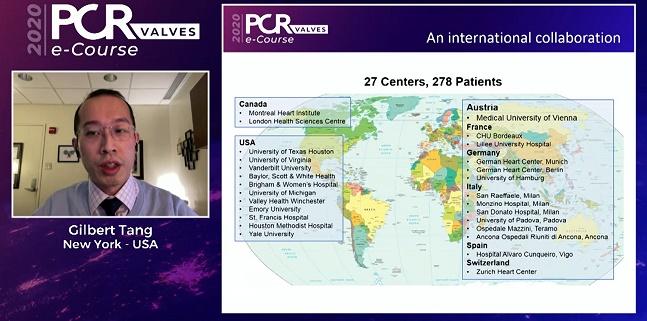
Gilbert Tang, MD, MSc, MBA (Mount Sinai Health System, New York, NY), presented the data this week during the PCR Valves e-Course, stressing that the registry includes some of the earliest patients treated with the MitraClip (Abbott), back in 2005, as well as many of the world’s most-experienced centers. Notably, the registry is not tracking patients whose TEER procedures failed but who did not or could not undergo subsequent surgeries to fix the problem. CUTTING-EDGE only includes the patients in whom surgery was deemed to be an option, making it a “highly selected” group.
“One of the key points is that this is the first study of its kind to look at this in a large number of centers, and a large number of patients, in a truly international collaboration,” Tang told TCTMD. “Right now we're still learning as we digest the data and trying to understand the implications. There will be more and more questions raised about outcomes after TEER, when they fail, and what to do with them. This is just scratching the surface.”
Over 100,000 TEERs have been performed internationally for symptomatic moderate-to-severe mitral regurgitation (MR), but multi-institutional, longitudinal data on MV surgery after TEER are lacking, Tang said. The current analysis from CUTTING-EDGE, which includes a patient treated as recently as November 2020 as well as some of the earliest patients to undergo clip repair, provides one of the first snapshots of how patients do when they need reinterventions. In all, 278 patients from 27 centers over a 15-year period were included in the study.
Procedural Details
The mean age of the patients in the registry was 73—relatively young, compared with the patient population undergoing TAVR, Tang observed. Median STS score was 5, and he reminded his virtual audience that anything over STS 6 is considered to be prohibitive surgical risk. Nearly 60% were treated with the first-generation MitraClip, and 56% had degenerative or mixed mitral valve disease. The median interval from TEER to surgery was 4.8 months: in 16.1% of patients these were aborted clip procedures, meaning that they headed for surgery as quickly as possible, while acute failure occurred in 18% of patients and was “delayed” in 66%.
Reasons for surgery were varied, with recurrent MR being the most common at 40%, followed by leaflet detachment in 34%, residual MR in 29%, and mitral stenosis in 15%. Not surprisingly, MV replacement surgery was far and away the most common procedure, done in more than 95% of cases. To TCTMD, Tang pointed out that the clip is typically “healed” in place after 6 weeks, making it very difficult to remove and still have enough tissue left for surgical leaflet repair, particularly for functional MR. “So rather than spending a lot of time trying to repair the valve, it is more feasible to replace it,” he said.
Of note, 42% of patients also had concomitant tricuspid surgery; mean cardiopulmonary bypass and cross-clamp times were 136 and 84 minutes, respectively. “So these are not short surgeries,” Tang said.
Different Pathology, Different Outcomes
The chief aim of the analysis was to compare outcomes according to the underlying valve pathology, Tang told TCTMD, noting that previously published work by Paul Sorajja, MD (Abbott Northwestern Hospital, Minneapolis, MN), and colleagues points to better survival post-TEER in patients with degenerative MR (DMR) versus those with functional MR (FMR).
In CUTTING-EDGE, surgery for recurrent MR following TEER was more common in DMR patients than in FMR (41.5% vs 23.7%; P = 0.021). FMR patients had a shorter interval from TEER to surgery, shorter cardiopulmonary bypass times, and shorter cross-clamp times as compared with DMR patients, but they also had longer hospital stays—all statistically significant differences. “They do struggle a bit more post-op,” Tang said—not surprising since this is typically a sicker group.
And while operative mortality was very low overall, he continued—which underscores the feasibility of surgical do-overs, in expert hands—the later picture wasn’t particularly rosy. Overall 30-day and 1-year mortality was “not trivial” at 13.4% and 25.5%, respectively, with signs that FMR patients fare worse over the longer term. At 3 years, survival for the cohort as a whole was around 70%, but that varied according to underlying pathology, reaching 77% in the DMR patients versus 58% for the FMR patients.
Subsequent analyses showed that a key predictor of 30-day and 1-year mortality, across the board, was presence of severe tricuspid regurgitation (TR). And it didn’t matter, Tang said, whether the TR was preexisting before the clip, developed after the clip, before the surgery or after the surgery. “So this is a very interesting finding.”
Plan Ahead
Jeroen Bax, MD (Leiden University Medical Center, the Netherlands), one of the session moderators, zeroed in on the TR finding following Tang’s presentation. “What always strikes me in all these studies that we do regarding the mitral valve, focusing on the left ventricle, [is that] the key driver—and you showed this also—is usually the right ventricle plus the TR. That’s an important thing for us to keep in mind. If that doesn’t function very well then you have a real chance of a not-so-good outcome.”
Anna Sonia Petronio, MD (Azienda Ospedaliero Universitaria Pisana, Pisa, Italy), the co-moderator, agreed, saying it’s important to understand that the impact of a failed TEER is “heavy.”
“You need . . . to think about it before performing percutaneous repair to understand what will happen to the patients later on, if you don’t succeed,” she said.
Indeed, that’s a key point, said Tang to TCTMD, emphasizing that these results were seen at high-volume centers, representing the “best-case scenario.”
“The key thing to take away from this data is that surgery after failed edge-to-edge repair carries some risks,” he said. “The heart team discussion for patients who are being evaluated for edge-to-edge repair should be taking into consideration the likely success of 1+ or less residual MR at the end to avoid surgery later on, which would likely result in a replacement.”
And while he expects outcomes in recent years have gotten better and better—reflecting newer-generation devices and better implantation and surgical techniques—any gains will be offset by the fact that more and more TEER procedures are happening around the world, including at centers with lower volumes, developing skill sets, and less expertise in patient selection.
“Going forward, as MitraClip and other edge-to-edge repair therapies expand, we need to be very cognizant of the anatomy that is being considered for clipping,” he said, and be absolutely sure that a clip is the best initial choice, even in patients at high risk for surgery.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Tang GHL. Outcomes of mitral valve surgery after transcatheter edge-to-edge mitral valve repair: the CUTTING-EDGE registry. Presented at: PCR Valves 2020. November 22, 2020.
Disclosures
- Tang reports being a consultant for Abbott, Medtronic, and WL Gore.


Comments