Dapagliflozin Wins in Patients With CKD
The DAPA-CKD trial shows that the SGLT2 inhibitor improves renal and CV outcomes, and that it reduces mortality.
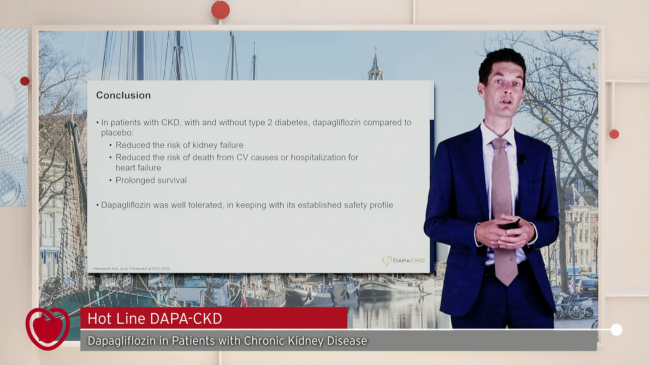
Regardless of diabetes status, patients with chronic kidney disease (CKD) have better renal and cardiovascular outcomes as well as a lower chance of dying when dapagliflozin (Farxiga; AstraZeneca) is added to standard-of-care therapies, the DAPA-CKD trial shows.
The composite primary outcome of a ≥ 50% decline in estimated glomerular filtration rate (eGFR), end-stage kidney disease, or renal or CV death was less frequent in patients treated with dapagliflozin versus placebo (HR 0.61; 95% CI 0.51-0.72), Hiddo Heerspink, PharmD, PhD (University Medical Center Groningen, the Netherlands), reported during the virtual European Society of Cardiology (ESC) Congress 2020. The number needed to treat was 19.
A range of renal outcomes were improved, and all-cause mortality was a relative 31% lower through a median follow-up of 2.4 years in the dapagliflozin arm (HR 0.69; 95% CI 0.53-0.88). Of particular interest to cardiologists, the composite of CV death or hospitalization for heart failure was reduced by a relative 29% (HR 0.71; 95% CI 0.55-0.92), similar to what was seen in the DAPA-HF trial of patients with chronic heart failure and reduced ejection fraction (HFrEF).
“The DAPA-CKD trial has shown dapagliflozin’s potential as a long-awaited new treatment option for patients with chronic kidney disease,” who are at high risk for adverse kidney and CV outcomes, Heerspink said during a press briefing.
CREDENCE, which evaluated canagliflozin in patients with type 2 diabetes and nephropathy, provided findings similar to those seen in DAPA-CKD, but this study of dapagliflozin is novel in that about one-third of patients did not have diabetes. These patients derived the same benefits as their diabetic peers, “which I think is a game changer,” said Rangaswami, who is vice chair of the American Heart Association’s Council on the Kidney in Cardiovascular Disease.
DAPA-CKD
Dapagliflozin and other SGLT2 inhibitors were initially developed as medications for type 2 diabetes, but their beneficial effects on renal and cardiovascular outcomes—even in patients without diabetes—have become clear. DAPA-HF with dapagliflozin and EMPEROR-Reduced with empagliflozin (Jardiance; Boehringer Ingelheim/Eli Lilly)—the latter reported at ESC 2020—both demonstrated benefits in the HFrEF population.
Across the SGLT2 inhibitor trials, positive signs have been seen for kidney outcomes, and DAPA-CKD was designed to better evaluate the renal effects of dapagliflozin. The trial, conducted at 386 sites in 21 countries, included 4,304 patients with chronic kidney disease (eGFR 25 to 75 mL/min/1.73 m2); their mean age was 62, and 33% of participants were women. Nearly all patients (97%) were on an ACE inhibitor or ARB at baseline.
On March 26, 2020, the trial’s independent data monitoring committee recommended stoppage of enrollment because of “overwhelming efficacy.”
Each component of the primary outcome was numerically lower with dapagliflozin versus placebo, reaching significance for a ≥ 50% decline in eGFR (HR 0.53) and end-stage kidney disease (HR 0.64). There were 65 CV deaths with dapagliflozin and 80 with placebo (HR 0.81; 95% CI 0.58-1.12). The numbers of renal deaths were two and six, respectively.
An outcome consisting of the renal endpoints only was reduced by a relative 44% with dapagliflozin (HR 0.56; 95% CI 0.45-0.68). The need for chronic dialysis was also lower in that arm (HR 0.66; 95% CI 0.48-0.90).
The results were consistent across subgroups, including in patients with or without type 2 diabetes.
Moreover, the treatment was well tolerated, Heerspink reported. Serious adverse events occurred in 29.5% of patients treated with dapagliflozin and 33.9% of those treated with placebo. Major hypoglycemia was less frequent in the dapagliflozin group (0.7% vs 1.3%). Of note, Heerspink said, there were no major hypoglycemic events in patients without diabetes. Diabetic ketoacidosis was seen in only two patients, both of whom were in the placebo arm of the trial.
Uniting Cardiologists and Nephrologists
Serving as a discussant after Heerspink’s presentation, Diederick Grobbee, MD, PhD (University Medical Center Utrecht, the Netherlands), said dapagliflozin’s safety profile “is indeed . . . good news for patients with chronic kidney disease.”
He pointed out, too, that the far-reaching benefits of the SGLT2 inhibitor were seen on top of standard-of-care therapy with ACE inhibitors and ARBs. “You may wonder if this is indeed the way to go, drug on drug on drug,” he said. “Or at some point we might wish to perhaps replace one for another that’s more beneficial, but that’s for future research.”
Rangaswami also said “the safety signal was fairly reassuring” in DAPA-CKD, but added that there is a risk of genitourinary infections because of the glucose loss inherent to SGLT2 inhibition. “That is something to keep in mind, and I think any patient, including those with kidney disease, should be aggressively counseled about that,” she advised.
She predicted that ACE inhibitors and ARBs would remain standard of care for patients with chronic kidney disease, but indicated that SGLT2 inhibitors had earned a place at the treatment table.
“I do think this will definitely become one of the standard-of-care therapies to be added on in patients on these renin-angiotensin-system inhibitors,” she commented. “And certainly, while people will keep these in mind, definitely more for the diabetic patients, I think we will now start using them in the nondiabetic CKD patients, which also make up a fair amount of the typical nephrologist’s practice.”
Taking a broader view, Rangaswami said she sees the positive SGLT2 inhibitor data as bringing the specialties of cardiology and nephrology even closer together. The heart failure trials have shown renal benefits and the kidney trials have shown cardiovascular benefits, she noted.
“It almost becomes less important who is actually primarily taking care of the patient with cardiorenal disease,” Rangaswami said. “It is almost like a heart failure specialist will be involved in treating the kidneys as a nephrologist will be involved in treating the heart. So I really think this has unified the two specialties—that’s never really happened before.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Heerspink H. DAPA-CKD: dapagliflozin in patients with chronic kidney disease. Presented at: ESC 2020. August 30, 2020.
Disclosures
- The trial was funded by AstraZeneca.
- Heerspink reports being a consultant to AbbVie, AstraZeneca, Bayer, Boehringer Ingelheim, Chinook, CSL Pharma, Gilead, Janssen, Merck, Mundi Pharma, Mitsubishi Tanabe, Novo Nordisk, and Retrophin and having received research support from AbbVie, AstraZeneca, Boehringer Ingelheim, and Janssen.
- Grobbee reports research grants, consulting fees, and travel reimbursement from AstraZeneca, Bayer, the Dutch Cancer Foundation, the Dutch Medical Research Council (ZonMW), the European Union, the FDA, IMI, Nestle, the Netherlands Heart Foundation, MSD, NIH, NHLBI, Novo Nordisk, Organon, Pfizer, Roche, the Royal Dutch Academy of Sciences, Sanofi, Servier, St, Jude, Unilever, Vifor, the Wellcome Trust, and Whyett.
- Rangaswami reports no relevant conflicts of interest.


Comments