DISRUPT CAD III: Lithotripsy Boosts Stent Expansion in Highly Calcified Lesions
“Jaw-dropping” and “spectacular” were some of the adjectives describing the calcium-cracking in early, nonrandomized results.
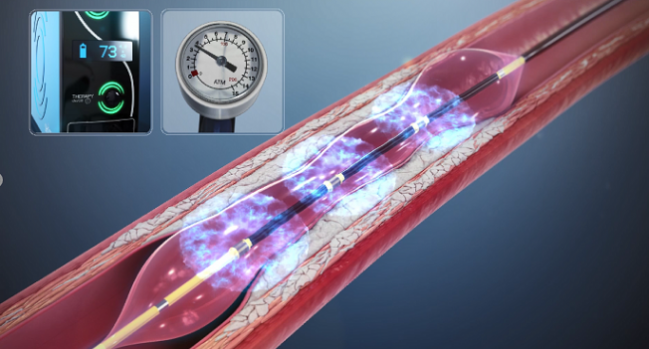
(UPDATED) Coronary intravascular lithotripsy shows promise for improving the ability to optimize PCI in severely calcified lesions, with good safety and efficacy out to 30 days, according to data from the single-arm DISRUPT CAD III trial.
In a press conference prior to his presentation during TCT Connect 2020, Dean Kereiakes, MD (The Christ Hospital Heart and Vascular Center, Cincinnati, OH), called the amount of calcification among the trial participants “staggering.” The average calcified segment length was 48 mm, all were graded as severely calcified by the core lab, and 30% had side-branch involvement. As Kereiakes showed, the procedure, which involves using acoustic pressure waves to fracture calcium, was well tolerated, with low rates of clinical and angiographic complications.
Speaking with TCTMD, he said the results were better than expected, especially in the historical context that about 50% of stents placed in calcified vessels are under expanded.
“We were able to get 102% stent expansion on average in the area of maximum calcification,” Kereiakes said. “It's kind of jaw-dropping, and I don't know any other technology that could achieve that.” Longer-term clinical follow-up will be required to assess late outcomes, he added.
In light of the elevated risk of inadequate stent outcomes in this challenging patient population, press conference panelist Allen Jeremias, MD (St. Francis Hospital, Roslyn, NY), said finding new ways to crack the calcium and obtain optimal stent expansion is critically important.
“The success rate is high. I think it's relatively easy to use, as demonstrated, and I think the results are spectacular,” he observed. Jeremias also noted that the study authors conducted systematic intravascular imaging before and after the procedure, allowing for insight into how much stent expansion was achieved.
“I think this is a very important piece of the puzzle [for] a mechanistic understanding of how the technology works and what we can achieve with it,” he said.
Exceeding Performance Goals
DISRUPT CAD III enrolled 431 patients at 47 sites in four countries. All had stable, unstable, or silent ischemia and severely calcified de novo coronary artery lesions ≤ 40 mm in length with reference vessel diameters of 2.5 to 4.0 mm.
In half of all procedures, target lesion pre-dilatation was performed. The mean number of pulses delivered per procedure with the intravascular lithotripsy device (Shockwave Medical) was 68.8. Approximately one in five cases included post-dilatation following the intravascular lithotripsy, and nearly all stent placements were post-dilatated.
The primary safety endpoint of freedom from 30-day MACE was observed in 92.2% of patients, exceeding the performance goal. Similarly, the primary effectiveness endpoint for procedural success occurred in 92.4%, exceeding the performance goal.
By 30 days, MACE occurred in 7.8% of patients, and TLF in 7.6%, driven primarily by periprocedural MI. Two cardiac deaths occurred over the same period; one in the hospital after emergency surgery for abrupt coronary closure associated with failed stent delivery and a second after discharge due to STEMI complicated by cardiogenic shock associated with target-vessel, non-target lesion thrombosis distal to the stent.
ARC-defined definite or probable stent thrombosis occurred in three patients within 30 days, with all related to stent under-expansion or mid-stent filling defect.
At 30 days, 72.9% of patients were in NYHA class 0 compared with 12.6% at baseline.
Angiographic data showed postprocedural in-stent residual stenosis < 50% in all lesions, with < 30% residual stenosis in 99.5% of lesions. The final in-stent residual stenosis was 11.9%, with acute gain of 1.7 mm. Freedom from serious angiographic complications following intravascular lithotripsy and at any time point during the procedure were 97.4% and 96.9%, respectively.
Due to reports of transient ventricular capture or “shocktopics” during intravascular lithotripsy therapy, the study evaluated the frequency and clinical correlates of this phenomenon. While there were more instances of decreased systolic BP during the intravascular lithotripsy in patients with transient ventricular capture compared to those without (40.5% vs 24.5%, P = 0.0007), the magnitude of the decrease was similar in both groups. Additionally, ventricular capture was not associated with sustained ventricular arrhythmias during or immediately after the procedure, nor did it correlate with adverse events.
Given the lack of a comparator arm, Kereiakes said performance goals for DISRUPT CAD III were designed in conjunction with the US Food and Drug Administration based on ORBIT II, a single-arm, nonrandomized IDE trial of orbital atherectomy. However, he noted that target-lesion complexity in DISRUPT CAD III was significantly greater.
There were no perforations seen in the trial, and Kereiakes said the device itself is simple for operators to use. Nevertheless, while imaging is not required, he said optical coherence tomography and calcium volume index may help when confronted with heavily calcified vessels. While the trial did not allow the use of scoring/cutting balloons or atherectomy, Kereiakes said they also are “absolutely complementary” and could be incorporated in cases of deep calcium.
Following the presentation, panelist Anthony Gershlick, MD (Glenfield Hospital, Leicester, England), noted that he has observed some balloon perforations associated with the intravascular lithotripsy device even at low pressures (< 4 atm).
Kereiakes acknowledged that while he also has seen some perforations in prior series, those occurred before the balloon material was changed and were not an issue in DISRUPT CAD III.
Photo Credit: Kereiakes DJ. Intravascular lithotripsy for treatment of severely calcified coronary artery disease: the Disrupt CAD III study. Presented at: TCT Connect 2020. October 15, 2020.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Hill JM, Kereiakes DJ, Shlofmitz RA, et al. Intravascular lithotripsy for treatment of severely calcified coronary artery disease: the DISRUPT CAD III study. J Am Coll Cardiol. 2020;Epub ahead of print.
Disclosures
- The study was funded by Shockwave Medical.
- Hill reports receiving fees and grant support from Abbott Vascular, Boston Scientific, Abiomed, and Shockwave Medical and being a stockholder in Shockwave Medical.
- Kereiakes reports consulting for SINO Medical Sciences Technologies, Inc., Boston Scientific, Elixir Medical, Svelte Medical Systems, Inc., Caliber Therapeutics/Orchestra Biomed, and Shockwave Medical; and being a stockholder in Ablative Solutions, Inc.
- Jeremias reports consultant fee/honoraria/speaker's bureau fees from Abbott Vascular, Boston Scientific, Volcano, and ACIST.
- Gershlick reports no relevant conflicts of interest.


Comments