FLAVOUR: FFR as Good as IVUS for Intermediate Coronary Stenoses
At 2 years, there was no difference in the primary outcome, but the FFR-guided strategy led to fewer stents being implanted.
WASHINGTON, DC—A head-to-head comparison of two imaging modalities—one assessing physiology, the other anatomy—suggests that both are equivalent when used to guide treatment of patients with intermediate coronary stenoses.
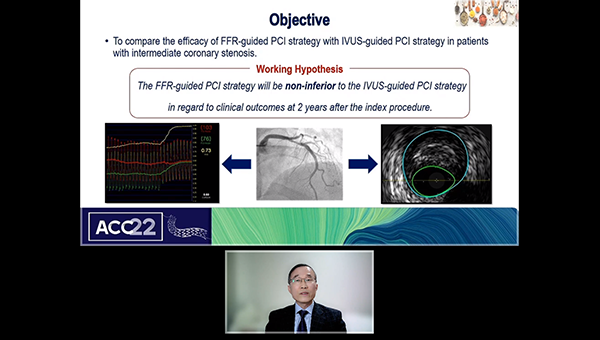
In FLAVOUR, presented as a late-breaking clinical trial at the American College of Cardiology 2022 Scientific Session, fractional flow reserve (FFR)-guided PCI was noninferior to IVUS-guided PCI in terms of hard clinical outcomes at 2 years. Moreover, use of physiology-based imaging with FFR led to fewer stents being implanted.

In terms of selecting the ideal strategy for patients with intermediate stenoses, operators should first start with FFR to determine if PCI is even necessary, say researchers.
“The textbook answer is to start with physiology,” lead investigator Bon-Kwon Koo, MD, PhD (Seoul National University Hospital, Korea), said when asked about the clinical implications of the study. “If you have to do PCI, IVUS-guided PCI or imaging-guided PCI should be performed. [From a] practical point of view, it’s not easy to use both, so our study is saying that for the intermediate coronary stenosis . . . if you have to choose one, you better choose physiology, although the best might be using both imaging and physiology. That’s my message from the trial.”
Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), the discussant following the late-breaking presentation, called FLAVOUR a “phenomenal study,” one that tacitly acknowledged in its design that angiography alone is not enough for intermediate coronary lesions.
“The fact that they studied physiology and imaging suggests that we need to do more than just looking at the angiogram,” said Kirtane.
However, he questioned testing the “exclusivity of modalities,” that being FFR versus IVUS, because practice has evolved such that operators use physiology to determine when or when not to treat and imaging then to optimize the procedure if it goes forward. Koo agreed with the premise of Kirtane’s question but argued that in many centers both physiology- and imaging-guided modalities might not be available to operators.
“In general, PCI practitioners may be pushed to use one,” said Koo.
Fewer Stents Implanted with FFR
The FLAVOUR trial—an investigator-initiated, prospective, randomized, noninferiority study—randomized 1,682 patients suspected to have ischemic coronary disease and an intermediate stenosis on angiography (40% to 70%). The indications for PCI included an FFR ≤ 0.80 for the 838 patients enrolled in the physiology-guided arm and a minimum lumen area (MLA) ≤ 3 mm2 (or MLA > 3 but ≤ 4 mm2 plus plaque burden > 70%) for the 844 patients enrolled in the IVUS arm.
In the FFR-guided arm, 44.4% of patients underwent PCI compared with 65.3% in the IVUS arm (P < 0.001).
The primary outcome, which was a patient-oriented composite endpoint that included death from any cause, MI, and any revascularization at 24 months, occurred in 8.6% and 8.1% of the IVUS and FFR groups, respectively (P = 0.015 for noninferiority; noninferiority margin 2.5%). There were no differences in any of the individual components of the primary endpoint. In terms of patient-reported outcomes, there was no difference in Seattle Angina Questionnaire scores between those randomized to FFR and IVUS.
Stratifying the groups based on the treatment received, there was no difference in the primary endpoint among those randomized to FFR or IVUS who were treated with medical therapy. For those who were stented, there was a trend toward fewer primary endpoint events in the IVUS group, but the difference did not reach statistical significance.
Finally, the investigators also looked at clinical outcomes based on whether PCI was “optimized.” In the FFR group, where 50.1% of stents were optimally placed, the primary endpoint occurred in 12.3% of FFR-optimized PCIs, 11.8% of suboptimal PCIs, and in 5.0% of those who received medical therapy based on the FFR data. Comparatively, in the IVUS arm, where 54.8% of PCIs were optimized, the primary endpoint occurred in 8.5% of optimized PCIs, 9.8% of suboptimal PCIs, and in 5.9% of those treated with medical therapy.
Speaking with the media, Frederick Welt, MD (University of Utah School of Medicine, Salt Lake City), said FLAVOUR will have an important impact on how interventionalists approach patients with angiographically-indeterminate coronary lesions.
“I think the major message here is that the group that had FFR had dramatically lower rates of revascularization,” said Welt. “If you pair that with no difference in the primary outcome, it’s hard to say that this shouldn’t be the way that we choose patients. With intravascular ultrasound, a much higher proportion of patients go on to PCI. I think this confirms what a lot of us feel about the two technologies, that FFR is much better at that sort of discrimination.”
Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York), who spoke with the media about the results, said that with equivalent clinical outcomes at 2 years, but significantly fewer stents, FLAVOUR is “really telling me that [FFR guidance] is the way to start, at the very least.”
One, the Other, or Both?
FLAVOUR is a good news story, added Mehran, something the FFR field needed after FAME 3 study and some other recent trials. She pointed out that physicians do not frequently use FFR to optimize stent implantation but will instead turn to IVUS or other imaging-based modalities. Additionally, using IVUS to determine lesion significance is a novel hypothesis.
Welt made a similar observation, adding that he thinks “FRR should be used to decide who gets an intervention and IVUS should be used to optimize the intervention.” He added that roughly 30% of the study participants had ACS, and there’s some “discomfort” amongst interventionalists in using FFR in the ACS setting.
Finally, Mehran highlighted the very low clinical event rate in the FFR-randomized patients treated with medical therapy, noting that it was even lower than among those who received optimal stent placement with IVUS.
“Deferring patients based on FFR guidance is extremely safe and associated with very low events,” she said.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Koo B-K. Fractional flow reserve versus intravascular ultrasound to guide percutaneous coronary intervention: the FLAVOUR trial. Presented at: ACC 2022. April 4, 2022. Washington, DC.
Disclosures
- Boston Scientific provided a research grant to fund the FLAVOUR trial, but had no role in trial design, data collection, analysis, or interpretation.
- Koo reports research grants from Abbott, Boston Scientific, and Philips Volcano






Comments