FAME 3: PCI Fails to Demonstrate Noninferiority to Surgery in Three-Vessel CAD
Interventionalists and surgeons call it a big win for CABG surgery, especially since its advantages were seen so early.
(UPDATED) In a head-to-head comparison of two revascularization strategies for patients with three-vessel coronary artery disease, PCI guided by a functional assessment of ischemia using fractional flow reserve (FFR) failed to match CABG surgery for the reduction of major adverse cardiovascular and cerebrovascular events.
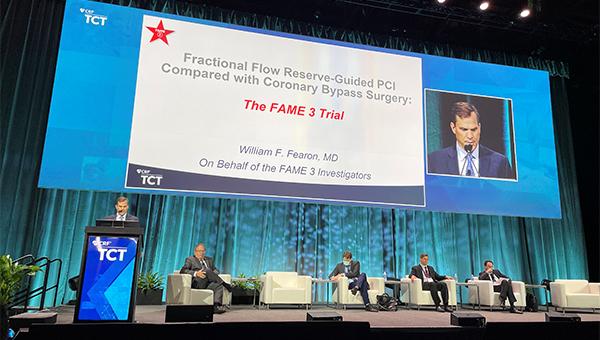
In the FAME 3 study, presented at TCT 2021 and published simultaneously in the New England Journal of Medicine, patients treated with FFR-guided PCI had a higher rate of death from any cause, MI, stroke, or repeat revascularization that those treated with surgery, missing the noninferiority margin established by investigators.
Regarding the primary endpoint’s individual components, there were no significant differences between PCI and CABG, although event rates, aside from stroke, were numerically higher with PCI. Patients with less-complex CAD, those with a low SYNTAX score (< 23), fared better with PCI than with CABG surgery, but investigators caution that the subgroup analysis is hypothesis-generating only.
“This study provides both physicians and patients more contemporary data and information on options and expected outcomes in patients with multivessel disease,” said lead investigator William Fearon, MD (Stanford University School of Medicine, CA), during a press conference announcing the results. “If you’re a patient with less-complex disease, I think you can feel comfortable that you will get an equivalent result with FFR-guided PCI. If you have more-complex disease, at least based on the outcomes here, which included repeat revascularization, bypass outperformed PCI.”
Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), who moderated the press conference, challenged that interpretation, saying that it’s troubling to view the subgroup analyses positively in light of FAME 3 missing the noninferiority margin on the primary endpoint. The study failed to demonstrate noninferiority, she stressed, and all subsequent analyses should thus be considered hypothesis-generating.
“It’s an observation that would require prospective randomized trials to validate,” said Mehran. Fearon, for his part, conceded that the observed benefit in patients with a low SYNTAX score should be considered a hypothesis at this point.
Patrick Myers, MD (Lausanne University Hospital, Switzerland), secretary-general elect of the European Association for Cardio-Thoracic Surgery (EACTS), said the FAME 3 clinical trial confirms the primacy of CABG surgery when compared against the most up-to-date PCI technologies.
“This was a well-conducted, investigator-initiated randomized, controlled trial,” Myers told TCTMD. “The rationale was very reasonable, and I think the investigators should really be commended for what they did. The results are striking. If we take the evidence from this trial, as well as from previous trials, it’s a very convincing result that confirms the superiority of CABG versus PCI in three-vessel coronary artery disease.”
Additionally, Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said FAME 3 upholds the standard of care for patients with three-vessel CAD. “Patients should be taken off the table, and we should discuss the treatment with surgeons,” he told TCTMD. “Also, this is just 1-year data and if any prior studies are predictors of what will happen, the [event] curves will spread over time, particularly for those higher-complexity patients. If at 1 year there is already this benefit of surgery, I think that’s pretty supportive of a surgical approach in these patients.”
In the US guidelines for the treatment of stable ischemic heart disease, CABG is a class 1 recommendation (level of evidence B) for the treatment of patients with three-vessel disease, with the guidelines stating “it is reasonable” to choose CABG over PCI in patients with complex three-vessel CAD (SYNTAX score > 22) who are good candidates for surgery. PCI, in this setting, is a IIb recommendation, meaning it is “of uncertain benefit.”
With the European guidelines for myocardial revascularization, PCI is a class 1A recommendation for the treatment of patients with three-vessel disease and a low SYNTAX score (≤ 22). For those with an intermediate-to-high SYNTAX score, however, PCI is not recommended (class III). In contrast, CABG surgery is a class 1A recommendation in patients regardless of SYNTAX score.
PCI Guided by FFR
The FAME trials testing the use of FFR in different clinical scenarios go back more than a decade. In 2009, the FAME trial showed that FFR-guided PCI reduced the risk of all-cause mortality, MI, or repeat revascularization when compared with angiography-guided PCI. In FAME 2, a trial that was stopped early, FFR-guided PCI plus optimal medical therapy was superior to medical therapy alone in patients with stable ischemic heart disease, a benefit that was driven by a lower rate of urgent revascularization.
That set the stage for the FAME 3 study, a noninferiority trial that included 1,500 patients with three-vessel coronary artery disease randomized to CABG surgery or PCI guided by FFR. All patients had angina and/or evidence of myocardial ischemia and were amenable to either surgery or PCI as determined by the heart team. Patients with left main CAD were not included in the study. With PCI, patients were treated with the Resolute Integrity zotarolimus-eluting stent (Medtronic) if the FFR measured ≤ 0.80, a value which indicates reversible ischemia based on the prior FAME studies.
At 1 year, the primary composite endpoint of death from any cause, MI, stroke, or repeat revascularization occurred in 10.6% of patients treated with FFR-guided PCI and in 6.9% of those treated with CABG surgery (HR 1.5; 95% CI 1.1-2.2), a difference that failed to demonstrate noninferiority of PCI. The composite endpoint of all-cause death, MI, or stroke occurred in 7.3% of those treated with PCI and 5.2% of the CABG-treated patients (HR 1.4; 95% CI 0.9-2.1).
On the other hand, the risk of major bleeding, arrhythmia, and acute kidney injury were higher with surgery.
With respect to the risk of MACCE according to the SYNTAX score, the composite primary endpoint among those with a low SYNTAX score occurred in 5.5% of those treated with PCI compared with 8.6% in the CABG arm. For those with intermediate and high SYNTAX score, the risk of death from any cause, MI, stroke, or repeat revascularization was higher among those treated with PCI.
Gregg Stone, MD (Icahn School of Medicine at Mount Sinai), who moderated the late-breaking clinical trial session, said he didn’t want to sound “like an apologist” for PCI but pointed out that the primary endpoint event rate was quite low, which necessitated adding repeat revascularization as part of the composite. For the hard endpoints—death, MI, or stroke—there was a smaller 2.1% difference favoring surgery, he noted.
Interventional cardiologist Ran Kornowski, MD (Rabin Medical Center, Petah Tikva, Israel), said FAME 3 shows that surgeons and interventionalists are achieving excellent results in patients with both strategies, “but better results with surgery, no doubt about it.” The subgroup analysis of patients stratified by SYNTAX score, he added, can be helpful in clinical practice, though long-term data beyond 1 year are needed before any conclusions can be drawn from that subanalysis.
‘I Was Wrong’
Marc Ruel, MD (University of Ottawa Heart Institute, Canada), said the results of the trial took him by surprise.
“Personally, I was wrong,” he told TCTMD. “I really thought that the 1-year results of FAME 3 would show noninferiority. I’d been saying this to many people because when you look at SYNTAX, FREEDOM, NOBLE, and EXCEL—the four main trials [comparing CABG versus PCI]—the event curves start separating at 2 to 3 years. In SYNTAX, there was no difference at 1 year. In EXCEL, there was no difference, same with NOBLE. In FREEDOM, it took 2 or 3 years for the curves to separate.”
Given the early separation of the event curves in FAME 3, Ruel, like Kirtane, expects the difference in clinical outcomes will be even more pronounced in long-term follow-up.
In terms of why FAME 3 failed to show PCI was noninferior to surgery, Ruel said surgeons are getting better at performing the procedure, with an increased focus on reducing the risk of adverse events, particularly the risk of stroke. The surgical techniques used by operators in FREEDOM and SYNTAX are now outdated, he added, noting that since those trials were published the surgical community has initiated sweeping quality-improvement initiatives.
“Surgeons have gotten their act together,” said Ruel. “There is no medical or surgical specialty, of all the specialties in medicine, that has their results as intensely scrutinized as cardiac surgery.” Today, greater attention is paid to limiting the risk of stroke and there is more emphasis on optimizing secondary prevention medications. As a result, clinical event rates in contemporary CABG trials are roughly half of what they were in FREEDOM and SYNTAX, he said.
With these improvements, and now these results from FAME 3, the data show that “stenting simply can’t match surgery,” said Ruel.
To TCTMD, Kirtane said the results hinting at better outcomes at 1 year with PCI in those with less complex CAD fits with his clinical experience.
“In general, there are surgeons where even if there is a three-vessel-disease patient with focal disease they’ll present PCI as an option,” he said. “And clearly, there is multivessel disease where I tell the patient that they need to have surgery and I won’t even entertain the notion of PCI. Clinicians in practice do this already, and they have a reasonable sense of what the outcomes would be. This data reaffirms what we do already know about multivessel disease and reaffirms the anatomic stratification of these patients, which is very important.”
Overall, FAME 3 showed that PCI still needs to improve, said Kirtane. While operators used modern stents with FFR guidance, use of intravascular imaging was low, he noted. Intravascular imaging was used in just 11.7% of PCI-treated patients, which is completely unacceptable in complex, multivessel disease, said Kirtane.
With respect to his clinical perspective, Ruel said that CABG should be the preferred approach for all “well-functioning” patients with multivessel CAD. “If I had a patient who wasn’t well functioning, had significant comorbidities, who wasn’t mobile, or who had a poor quality of life because of other ailments, then PCI has a very important role,” he said.
Challenging the Usefulness of FFR?
For Myers, the findings also call into question the benefits of using FFR to guide PCI, noting that the recent FLOWER-MI failed to show that use of the technology reduced the risk of clinical events compared with angiography-guided PCI. Adding FFR to diagnostic coronary angiography also didn’t provide any advantages in the RIPCORD 2 study.
“FFR has never really been shown to be useful in CABG, and [FAME 3] makes me wonder how useful it is in generally managing our patients,” said Myers.
Myers stressed the FAME 3 investigators were open in disclosing the rationale and methodology for the study, noting the study protocol was updated by the steering committee in 2019 following the publication of the BEST, EXCEL, and NOBLE clinical trials. Based on those trials, the 1-year predicted MACCE rate was thought to be lower than anticipated and this led the FAME 3 investigators to adjust the upper margin for the noninferiority hazard ratio from 1.45 to 1.65. In addition, the long-term follow-up was extended from 3 to 5 years.
Despite showing that PCI was not noninferior to CABG surgery, Myers believes the 1-year follow-up for the study’s primary endpoint is not sufficiently long enough, noting that invasive surgery carries with an up-front cost and that the benefits are borne out over time. Nonetheless, even at this early timepoint, the 3.7% absolute difference in the risk of primary endpoint clearly shows the advantages of CABG surgery in three-vessel CAD, said Myers.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Fearon WF, Zimmerman FM, De Bruyne B, et al. Fractional flow reserve-guided PCI as compared with coronary bypass surgery. N Engl J Med 2021;Epub ahead of print.
Disclosures
- The FAME 3 was funded by Medtronic and Abbott Vascular.
- Kirtane reports institutional funding to Columbia University and/or the Cardiovascular Research Foundation (CRF) from Medtronic, Boston Scientific, Abbott Vascular, Amgen, CSI, Siemens, Philips, ReCor Medical, Neurotronic, Biotronik, and Chiesi. In addition to research grants, institutional funding includes fees paid to Columbia University and/or CRF for consulting and/or speaking engagements in which Kirtane controlled the content. Kirtane also reports consulting from IMDS and receiving travel expenses/meals from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron.
- Mehran reports grant support/research contracts (institutional) from Abbott Vascular, AstraZeneca, Bayer AG, Bristol-Myers Squibb, CSL Behring, Daiichi-Sankyo/Eli Lilly and Company, Medtronic, Novartis Pharmaceuticals, OrbusNeich, CERC, Chiesi, Concept Medical, Applied Therapeutics, Beth Israel Deaconess, Zoll, Arena, Biosensors, Boston Scientific, CellAegis, Insel Gruppe AG, Philips, and Transverse Medical; consultant fees/honoraria/speakers bureau fees (personal) from Medscape/WebMD, Janssen Scientific Affairs, Cine Med Research, ACC, CIRM, SCAI, and WebMD; equity < 1% (personal) from Elixir Medical, Applied Therapeutics, and STEL; equity < 1% to her spouse (personal) from ControlRad; advisory board payments (institutional) from Idorsia Pharmaceuticals; scientific advisory board payments (personal) from the AMA; consultant fees/honoraria/speakers bureau fees (institutional) from Abbott Vascular, Abiomed, AM-Pharma, Alleviant, Bayer, Beth Israel Deaconess, CardiaWave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; divested equity < 1% (institutional) from Claret Medical (now Boston Scientific); and scientific advisory board payments to her spouse (personal) from Biosensors.




Comments