GUIDE-HF Hints That Hemodynamic-Guided Management Works in HFpEF
It’s a subgroup analysis from a study hindered by the COVID-19 pandemic, so the finding may be hypothesis-generating only.
Overall, rates of the trial’s primary endpoint were lower in patients with heart failure and preserved ejection fraction (HFpEF) than in those with reduced EFs, but hemodynamic-guided management with CardioMEMS—a device implanted into the pulmonary artery to measure changes in pressure that would warrant a change in care—resulted in a similar relative reduction in HFpEF patients and those with heart failure with reduced ejection fraction (HFrEF).
Lead investigator JoAnn Lindenfeld, MD (Vanderbilt University Medical Center, Nashville, TN), who presented the results of the subgroup analysis to the media at TCT 2021, said GUIDE-HF shows that “hemodynamic-guided management of heart failure is one of a very small number of effective therapies in HFpEF patients.”
Despite the favorable trends in HFpEF patients, there are important caveats to the study.
The relative reduction in risk of the primary endpoint, as well as the reduction in HF events, with pulmonary artery pressure monitoring was not statistically significant in the HFpEF or HFrEF subgroups, said Lindenfeld, but the subgroup analysis, while prespecified, was not sufficiently powered to detect meaningful differences. During the pandemic, there was a marked reduction in hospitalizations for HF, she noted, and they observed a significant interaction between the COVID-19 period and the primary endpoint—as previously reported by TCTMD. For that reason, this subgroup analysis focused solely on clinical events that occurred before COVID-19 wreaked havoc on the trial—a strategy also used to make sense of the main trial findings.
We believe there is a very consistent story here. JoAnn Lindenfeld
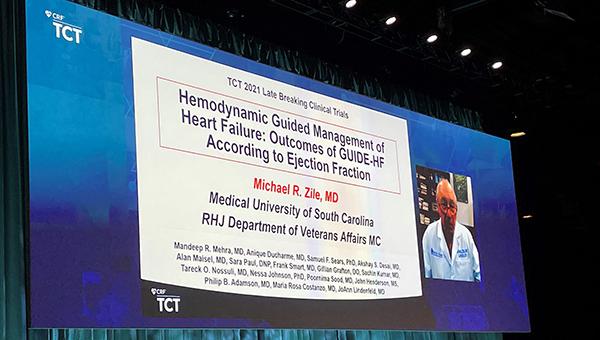
Even with those qualifications, the new analysis shows very consistent reductions in the risk of HF visits, as well as in the study’s primary endpoint, in patients with both HFpEF and HFrEF, according to investigators. Michael Zile, MD (Medical University of South Carolina, Charleston), who presented the subgroup analysis during the late-breaking clinical trial session, said that regardless of the EF cutoff used, they observed a reduction in clinical events in this broad population of HF patients.
“We believe there is a very consistent story here,” added Lindenfeld, noting that physicians will need to carefully scrutinize all the available data.
Other physicians, however, stressed that these new results from GUIDE-HF should be considered hypothesis-generating for now.
“This is a subgroup analysis of a trial that is already controversial because of the fact that they looked at data before COVID-19,” said Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, NY), who spoke with the media after the presentation. “The power of the study is diminished when you cut it earlier and it’s difficult to interpret. I’m not saying this is a positive or negative study—it’s interesting that the trends and relative risk reductions were similar for HFpEF and HFrEF. The next question is can we do a HFpEF study and see what type of intervention actually is making an important difference when using these types of devices.”
GUIDE-HF
In GUIDE-HF, investigators aimed to demonstrate that the CardioMEMS device could be used in a broader group of HF patients than in the pivotal CHAMPION trial of NYHA class III heart failure patients, a study that led to device approval in the US and Europe. In GUIDE-HF, which was published in the Lancet in August 2021, investigators tested whether the benefits of using the device could be expanded to patients with NYHA class II or IV heart failure, or to patients with elevated natriuretic peptides, but no prior hospitalization.
In total, 1,000 patients were implanted with the pulmonary artery pressure sensor between January and December 2019, then randomized to having their care informed by monitoring or to receiving standard-of-care management without access to sensor data. As reported by TCTMD, the trial missed its primary endpoint, but an analysis showed that COVID-19 had a significant effect on the results, which led researchers to focus only on clinical events that occurred before March 2020 when the US declared a national emergency. In that narrower window, hemodynamic-guided therapy with CardioMEMS significantly lowered the risk of the primary endpoint and HF events.
It’s an exciting area, and the bottom line is that sensor or not, there is room for tailored therapy. Mintu Turakhia
Speaking with the media, Lindenfeld explained that in patients with HFrEF and HFpEF, pulmonary congestion is a major cause of poor functional capacity, poor quality of life, HF hospitalizations, and increased mortality. Zile noted that it can be more difficult to determine volume status in HFpEF, especially in the ambulatory setting.
Focusing on clinical events during the pre-COVID-19 window, the subgroup analysis showed that the hemodynamic-guided strategy reduced the risk of all-cause mortality, hospitalizations, and urgent heart failure visits by 30% in HFpEF patients and by 15% in those with HFrEF, neither of which was significant. Similarly, use of CardioMEMS versus usual care reduced HF events by 28% and 23% in the HFpEF and HFrEF patients, respectively. Again, the reductions weren’t statistically significant.
In terms of what made the difference in HFpEF patients—a disease with limited therapies when compared with HFrEF—Lindenfeld said it was primarily a change in diuretic therapy based on hemodynamic guidance. In GUIDE-HF, she said, two-thirds of patients had their diuretic medication titrated upwards and one-third shifted down.
“There were fewer medication changes in HFpEF than in HFrEF, but I think that’s consistent with the fact that there are fewer heart failure hospitalizations and fewer episodes of congestion,” she said. “In general, the types of medication changes track the same—they are primarily diuretics for HFpEF and HFrEF.”
For Mintu Turakhia, MD (Stanford University School of Medicine, CA), who wasn’t involved in the study, GUIDE-HF is a difficult trial to interpret given the COVID-19 effect. Nonetheless, the study emphasizes the importance of determining the best stepwise approach for managing patients with HFpEF.
“Throwing on a diuretic and beta-blocker and starting to escalate several classes of antihypertensives is not the right approach,” he said. “There is something here about the congestion-guided approach, where you might need more diuretics than they’d ordinarily receive. It’s an exciting area, and the bottom line is that sensor or not, there is room for tailored therapy. There is going to be much more sequencing of heart failure therapy postdischarge because you can’t do it all in the hospital.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Zile MR, on behalf of the GUIDE-HF investigators. Hemodynamic-guided management of heart failure: outcomes of GUIDE-HF according to ejection fraction. Presented at: TCT 2021. Orlando, FL. November 6, 2021.
Disclosures
- Lindenfeld reports grant/research support from AstraZeneca, Volumetrix, Sensible Medical; and consulting fees/honoraria from Abbott, Allegiant, AstraZeneca, Boehringer Ingelheim, Boston Scientific, CVRx, Edwards Lifesciences, Merck, and VWave.
- Zile reports consulting fees/honoraria from Abbott Vascular.
- Turakhia reports institutional grant support/research contracts from Bayer, Bristol-Myers Squibb; equity/stocks/options from AliveCor and 100Plus; and consulting fees/honoraria from Medtronic, Biotronik, Abbott Vascular, Sanofi-Aventis, Myokardia, and Johnson & Johnson.
- Mehran reports grant support/research contracts (institutional) from Abbott Vascular, AstraZeneca, Bayer AG, Bristol-Myers Squibb, CSL Behring, Daiichi-Sankyo/Eli Lilly and Company, Medtronic, Novartis Pharmaceuticals, OrbusNeich, CERC, Chiesi, Concept Medical, Applied Therapeutics, Beth Israel Deaconess, Zoll, Arena, Biosensors, Boston Scientific, CellAegis, Insel Gruppe AG, Philips, and Transverse Medical; consultant fees/honoraria/speakers bureau fees (personal) from Medscape/WebMD, Janssen Scientific Affairs, Cine Med Research, ACC, CIRM, SCAI, and WebMD; equity < 1% (personal) from Elixir Medical, Applied Therapeutics, and STEL; equity < 1% to her spouse (personal) from ControlRad; advisory board payments (institutional) from Idorsia Pharmaceuticals; scientific advisory board payments (personal) from the AMA; consultant fees/honoraria/speakers bureau fees (institutional) from Abbott Vascular, Abiomed, AM-Pharma, Alleviant, Bayer, Beth Israel Deaconess, CardiaWave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; divested equity < 1% (institutional) from Claret Medical (now Boston Scientific); and scientific advisory board payments to her spouse (personal) from Biosensors.




Comments