Healed MI at the Root of Many Sudden Deaths: Autopsy Data
To “really make a dent” in fatalities, better risk stratification and a proactive approach are needed, one expert told TCTMD.

Healed myocardial infarction is common among people who suffer sudden death, far outnumbering acute MI, Norwegian autopsy data show. This distribution pattern is most apparent in men.
“It was not a surprise for us that myocardial infarcts explained a large proportion of sudden and unexpected deaths [43%], but it was a surprise that the proportion of healed infarcts (75% to 80%) was much higher than acute ones both in men and women,” lead author Bjørn O. Mæhle, MD, PhD (Gade Laboratory for Pathology, University of Bergen, Norway), writing on behalf of the team, told TCTMD via email.
Sumeet S. Chugh, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, CA), said the study adds incremental support to what’s known about the causes of cardiac arrest and sudden death. “It’s good to get autopsy data,” he agreed.
But there are many missing pieces, Chugh noted. For instance, there are no details on whether the healed cases represented “silent MIs” that went unrecognized prior to autopsy and are known to increase long-term mortality risk as much as acute MIs.
Moreover, focusing on heart muscle alone could skew the numbers, he commented to TCTMD. “If you had your heart attack a day or two before your autopsy was done, you may just have evidence in the coronary arteries and no evidence in the muscle. They may be really undercounting acute MI” or, on the flipside, mistaking myocarditis-related damage for an MI, Chugh observed. Nor is there information on the presence of left ventricular hypertrophy, also a risk factor for sudden death.
To “really make a dent” in fatalities, better risk stratification and a proactive approach are needed, urged Chugh. “The whole point of studying this is to reduce the burden of sudden cardiac death.”
Sex, Age Differences Seen
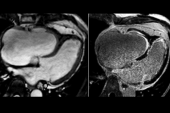
For their study, published as a research letter in the Journal of the American College of Cardiology, Mæhle et al examined records for 3,592 medicolegal autopsies of people (26% women) who died from natural causes between 1985 and 2004. Explaining how pathologists arrived at their diagnoses, the researchers explain that acute MI can lead to changes in cardiac muscle color. “A microscopic examination of the myocardium will show necrotic myocytes and sometimes also granulocytes,” they write, whereas “a healed MI appears as a well-defined scar consisting of connective tissue within the myocardium. At our laboratory, the pathologists record a healed MI as the cause of death if no other reasons are found.”
Four in 10 of the autopsies showed evidence of MI—fully 1,194 were healed and 252 were acute, with the rest being a combination of the two. In men, healed infarcts were fivefold more common than acute infarcts (78.8% vs 14.8%). In women, this scarring was three times more frequent than acute damage (69.3% vs 22.3%; P = 0.002 for interaction). Less than 10% of autopsies showed signs of both healed and acute MI.
There also were differences related to age among men, with healed infarcts linked to older age compared with acute infarcts (mean age 64.6 vs 61.9 years; P = 0.002). For women, the mean age was 71 in both groups, though the researchers note that there were a “relatively low number of MIs” among women.
“In view of the present and previous findings, there seems to be a need for increased knowledge of healed MI as a potential cause of death,” Mæhle and colleagues conclude. One biologically possible mechanism relates to fatal arrhythmias, they say. “A scar from a healed MI appears as an area of collagen fibrosis, in which cardiomyocytes and myofibroblasts with electrical conduction properties can be found. Formation of re-entry circuits in this area can lead to monomorphic ventricular tachycardias that can degenerate into ventricular fibrillation, with cardiac arrest and death as the outcome if untreated.”
The whole point of studying this is to reduce the burden of sudden cardiac death. Sumeet S. Chugh
To TCTMD, Mæhle suggested that “clinicians need to be aware of potential vague symptoms of a myocardial infarct, as well as potential sex differences in such symptoms, to be able to diagnose and treat the infarct.” For the healed cases, it might prove useful to monitor the “extent of scar tissue in the years after treatment of the infarct,” he said. “However, the knowledge on these issues is so far too limited to be directly applicable.”
Future research, said Mæhle, will require the adoption of standard protocols for recording infarct status on death certificates. Understanding the heart’s healing process and factors that predict prognosis post-MI are essential in preventing these deaths, he added.
Chugh agreed that there needs to be a rethink. “By the time somebody collapses in the street with a sudden cardiac arrest and they lose their pulse and someone calls 9-1-1, 90% of them are destined to die. . . . It’s too late for the vast majority,” he said, adding, “That’s why we’ve got to predict and we’ve got to prevent.”
As of now, the most commonly used predictor is left ventricular ejection fraction, Chugh noted. Below a certain LVEF cutoff, some patients are candidates for an implantable cardioverter-defibrillator. The problem, he continued, is that it “takes 30 to 99 defibrillators implanted in 1 year to save one life. We’re implanting so many defibrillators, but they’re not firing in most people.”
The current approach “is not sustainable, based on simple math,” stressed Chugh. “You can’t sustain this healthcare cost.”
On the other hand, most people who experience cardiac arrest don’t have a low ejection fraction, he pointed out. “So we need novel methods, [and] complicated problems need complicated solutions.” Clinical profiles, biomarkers, genetic factors, and cardiac arrest triggers are all under study. “That is where the field is going, and that’s what needs to be done,” Chugh concluded.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Mæhle BO, Barrett TM, Albrektsen G, et al. Acute and healed myocardial infarctions as cause of sudden death: age and sex differences. J Am Coll Cardiol. 2021:6;826-827.
Disclosures
- Mæhle reports no relevant conflicts of interest.
- Chugh reports funding from the National Institutes of Health.



Comments