iFR Matches FFR Through 5 Years: iFR-SWEDEHEART
For PCI guidance, both physiologic tests seem to be viable options, but each has their advantages and drawbacks.
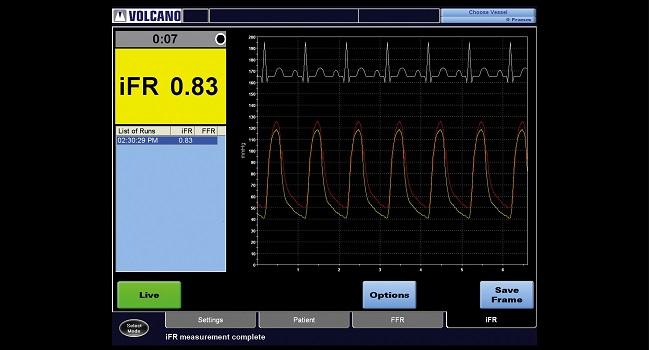
Photo Credit: Philips Healthcare
Final, 5-year data from iFR-SWEDEHEART, a Swedish registry-based RCT, confirm the continued safety and efficacy of using instantaneous wave-free ratio (iFR) compared with fractional flow reserve (FFR) to guide decisions on whether to revascularize.
iFR-SWEDEHEART’s initial results, along with those of the DEFINE-FLAIR trial, spurred debate over which form of physiologic testing is best. FFR involves using adenosine—which carries the risk of side effects and costs money, critics say—as well as measuring the pressure gradient across a lesion during hyperemia, whereas iFR is calculated during diastole and does not require use of hyperemic agents.
At 1 year, the main iFR-SWEDEHEART analysis showed iFR to be noninferior to FFR for the primary endpoint of MACE (death, nonfatal MI, and unplanned revascularization; P for noninferiority = 0.007, using a noninferiority margin of 3.2%). For many, the takeaway was a win for physiological assessment overall, not an endorsement of one test over another.
Matthias Götberg, MD, PhD (Skåne University Hospital, Lund University, Sweden), presented the latest data in a late-breaking clinical science session today at TCT 2021.
Most differences between iFR and FFR would be expected to occur within that first year, Götberg told TCTMD. Still, the researchers wanted to see whether those findings held up over time. In part, this was because “we had more lesions that were deferred, [or] not treated, when using iFR,” he said. “So for us it was very important to get that long-term follow-up data, to really show if there would be a later signal beyond 1 year.”
Although iFR-SWEDEHEART provides reassurance on the comparison of iFR versus FFR—specifically in patients with stable angina or NSTE ACS who had moderate stenosis on angiography, where revascularization’s value was ambiguous—other trials presented at TCT today may also have some bearing on physiologic-testing decisions.
For example, findings from this morning’s FAVOR III trial support a role for quantitative flow ratio (QFR), derived from angiography, which would allow for estimates of FFR without the use of a pressure wire or hyperemic drugs. On the other hand, FAME 3, also presented this morning, comparing FFR-guided PCI to CABG in multivessel CAD, failed to demonstrate noninferiority for the less-invasive strategy, leading some to question—on the backs of FLOWER-MI and RIPCORD—whether FFR actually holds the value that the earlier FAME trials suggested.
iFR-SWEDEHEART
iFR-SWEDEHEART randomized 2,037 patients taking part in the SCAAR registry who had 40% to 80% stenosis on visual assessment to iFR- or FFR-guided care. The threshold for revascularization (either PCI or CABG) was 0.89 for iFR and 0.80 for FFR; when values exceeded these prespecified cutoffs, treatment was deferred. Revascularization, most often PCI, was performed in 53.0% of the iFR group and 56.5% of the FFR group (P = 0.11).
iFR evaluated a higher mean number of lesions (1.55 vs 1.43; P = 0.002), but a lower proportion were functionally significant (29.1% vs 36.8%; P < 0.0001). For the patients who underwent PCI, the mean number of stents per patient was lower with iFR versus FFR (1.58 vs 1.73; P= 0.048).
Yet there was no difference in MACE rate by 1 year (6.7% for iFR and 6.1% for FFR; HR 1.12; 95% CI 0.79-1.58), and there were no differences regarding its components or the rate of stent thrombosis.
By 5 years, there had been no loss to follow-up. MACE rates were similar for iFR and FFR at 21.5% vs 19.9% (HR 1.09; 95% CI 0.90-1.33), as were rates of all-cause death, nonfatal MI, and unplanned revascularization. Subgroup analyses related to sex, age, comorbidities, smoking status, and angina symptoms showed no differences.
Evolutions in Physiologic Testing
Much has changed in the ensuing years since iFR-SWEDEHEART began enrolling patients, said Götberg. “When we started off, iFR was just a number—either you trusted iFR or you had to trust FFR. But we found that iFR was much quicker [to do] and it’s obviously easier to perform, and we found that it’s cheaper and [has] no side effects. So I think the adoption rate has really increased, because you lower the threshold for performing physiology.”
The technology’s use has continued to evolve, as well, with more pullbacks and greater use of SyncVision (Philips), “where we do a physical overlay of the pressure drop over the angio picture,” he added. The latter is now being evaluated by DEFINE GPS.
As to whether there’s any reason FFR might be preferred, Götberg replied: “I would say that iFR and FFR are both pressure indices—you choose one and you go by the numbers. But for me, I fail to see any additional information provided with FFR, to be honest.”
Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), moderating a TCT press conference, said that the large cohort and thorough follow-up of iFR-SWEDEHEART beg the question: “Do we just then use iFR? Why put the patients through FFR?”
“There are good reasons to do FFR,” replied Shmuel Banai, MD (Tel Aviv Medical Center, Israel), pointing to a wider scope of assessment. “When you do FFR you can . . . also do the whole physiology testing” that measures other parameters such as coronary flow reserve and index of microvascular resistance to study the microvasculature, “which is extremely important, because we miss that in about 50% of our patients. So until we have methods without a wire to measure microvascular function, when we do the testing, we do the FFR and the whole system.”
Mehran countered that this doesn’t undermine the findings of iFR-SWEDEHEART, where physiologic testing was used to look at borderline lesions and guide revascularization.
To TCTMD, Götberg said he sees no obvious downsides to iFR apart from it being a proprietary technology. “That’s the only limitation, . . . but other than that I think it fits the bill to be superior to FFR with [regard] to everything except for outcome,” he commented.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Götberg M. iFR-SWEDEHEART: Five-year outcomes of a randomized trial of iFR-guided vs. FFR-guided PCI. Presented at: TCT 2021. Orlando, FL. November 4, 2021.
Disclosures
- Götberg reports grant/research support from Boston Scientific and Philips Healthcare as well as consultant fees/honoraria from Abbott, Boston Scientific, and Medtronic.





Comments