IVUS, OCT Each Bring Something to the Table for PCI in Complex Lesions: Meta-analysis
Among various lesion subtypes, MACE risks were consistently lower with intravascular imaging vs angiography.

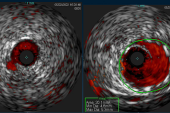
Intravascular imaging—whether that’s with IVUS or OCT—improves outcomes across various types of complex coronary lesions when used to guide PCI with drug-eluting stents, a network meta-analysis suggests.
Each of the modalities studied was associated with lower risk of MACE, defined as cardiac death, MI, or target vessel revascularization, compared with angiography in complex lesions as a whole. The two also held an edge individually in chronic total occlusions (CTOs), left main coronary artery disease, bifurcation lesions, multivessel coronary artery disease, and moderately or severely calcified lesions.
The paper was published recently in JACC: Cardiovascular Interventions.
Existing RCTs of intravascular imaging versus coronary angiography have, for the most part, enrolled patients with a variety of complex lesions and so were not powered to assess the individual features, lead author Pedro E.P. Carvalho, MD (Minneapolis Heart Institute Foundation, MN), told TCTMD. Thus, the researchers sought to understand whether “IVUS or OCT is better for a specific subtype of lesion.”
What the meta-analysis found is that IVUS and OCT each consistently offer benefits, he said. “There are some differences [between] the two. There are some lesions that are better assessed by IVUS. Some lesions are better assessed by OCT. But I think the main message here is that both of them are better than angiography to guide PCI, especially in the complex lesions.”
Moreover, the new study’s head-to-head comparisons between OCT and IVUS for individual lesion types showed no significant advantage for either, “so whichever you have available and you are more comfortable using should be your go-to,” Carvalho advised.
Daniele Giacoppo, MD, PhD (University of Catania, Italy), writing in an editorial, points out that randomized trials of intravascular imaging have generally found such guidance is linked to better clinical outcomes.
“However, when the totality of the accumulated evidence is critically reviewed, the magnitude and prognostic significance of these benefits vary substantially across trials,” he notes. “This heterogeneity in short- and long-term outcomes likely reflects differences in both the pattern and complexity of underlying coronary artery disease.”
During a memorable session reported on by TCTMD at the European Society of Cardiology Congress 2023, for example, the ILUMIEN IV and OCTOBER trials came to contradictory conclusions for OCT while the OCTIVUS trial found IVUS to be noninferior to OCT.
The new meta-analysis, Giacoppo says, “provides meaningful insights by showing consistent benefits of both IVUS and OCT over angiography alone across multiple types of complex coronary artery disease,” though he cautions that trials thus far have employed a mixed bag of designs and definitions for what constitutes complexity.
Two Strong Options
The investigators identified lesion-level data from 17 randomized controlled trials (n = 13,751 patients) on DES PCI of complex lesions. Around a third of cases involved IVUS, a quarter used OCT, and 43% used angiography alone.
Among all complex lesions, OCT guidance was linked to lower risk of MACE (RR 0.63; 95% CI 0.55-0.72) compared with angiography, as was IVUS guidance (RR 0.67; 95% CI 0.56-0.79), and MACE risks were similar between the two forms of intravascular imaging (RR 0.94; 95% CI 0.78-1.14). The same was true when looking individually at lesion types, though for CTOs, the advantage for OCT over angiography didn’t reach significance.
MACE Risk With Intravascular Imaging vs Angiography by Lesion Type
|
|
IVUS |
OCT |
|
Left Main |
0.52 (0.33-0.86) |
0.51 (0.30-0.86) |
|
CTO |
0.57 (0.38-0.88) |
0.61 (0.22-1.69) |
|
Bifurcation |
0.57 (0.39-0.85) |
0.70 (0.53-0.91) |
|
Moderately/Severely Calcified |
0.61 (0.38-0.98) |
0.66 (0.44-0.98) |
|
Long |
0.59 (0.46-0.75) |
0.73 (0.57-0.94) |
|
Multivessel |
0.55 (0.41-0.74) |
0.44 (0.30-0.64) |
Giacoppo, in his editorial, observes that IVUS and OCT diverge in terms of spatial resolution, tissue penetration depth, and technical requirements. In the setting of each lesion type, “these modality-specific distinctions have important implications for stent diameter and length selection, optimization of stent expansion and strut apposition, and early detection of dissections, plaque shift, and thrombosis,” he notes.
Carvalho and colleagues similarly draw attention to the two tools’ different capabilities. “It is critical,” they advise, “to consider the technical characteristics and procedural feasibility of intravascular imaging modalities when interpreting our findings across specific complex lesion subsets, as the utility of IVUS and OCT varies by lesion type.”
For example, in the CTO setting, “IVUS can facilitate proximal cap puncture, subintimal navigation, and reentry, whereas OCT is limited to postluminal crossing imaging,” they note. For left main disease, on the other hand, “IVUS remains the preferred modality because of its superior tissue penetration in large-caliber vessels.”
The investigators conclude that the meta-analysis bolsters the case for routine use of intravascular imaging guidance in high-risk lesions. That said, the tools’ “cost-effectiveness in noncomplex lesions remains insufficiently studied and warrants further investigation,” they caution.
“We know intravascular imaging is good for complex lesions,” Carvalho commented. “But what about lesions that are not complex, do we actually need to this? . . . Sometimes it’s a very simple lesion and you just deploy a stent there, and patients are going to be fine and you don’t necessarily need to use this technology.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Carvalho PEP, Antunes VLJ, de Pontes VB, et al. IVUS, OCT, or angiography as guidance for PCI in complex coronary artery lesions: network meta-analysis of randomized controlled trials. JACC Cardiovasc Interv. 2026;19:31-43.
Giacoppo D. Intravascular imaging to guide PCI for complex lesions: which lesions derive the greatest benefit from IVUS and OCT? JACC Cardiovasc Interv. 2026;19:44-46.
Disclosures
- Carvalho reports no relevant conflicts of interest.




Comments