Four Intravascular Imaging Studies Shared the ESC Spotlight, Yet Shadows Persist
Many hoped ILUMIEN IV and OCTOBER, plus an updated meta-analysis, would answer some questions. Instead they raised more.

AMSTERDAM, the Netherlands—Not for the faint of heart, an entire Hot Line session here at the European Society of Cardiology (ESC) Congress 2023 shone a spotlight on intravascular imaging (IVI) yet failed to fully clarify its role in PCI.
A new meta-analysis along with three randomized trials were presented in this high-profile session.
All showed that use of IVI, either optimal coherence tomography or intravascular ultrasound, led to better stent implantation, fewer complications, and less stent thrombosis. Two studies directly compared OCT to angiography for guiding PCI procedures, but only one of these delivered the hoped-for improvement in clinical events. The meta-analysis, however, combining patients from these two trials and 18 earlier studies, showed marked benefits with the use of IVI over traditional angiography across the spectrum of coronary lesions.
“The evidence really now is overwhelming,” said Gregg Stone, MD (Icahn School of Medicine at Mount Sinai, New York, NY), the final presenter of this session. “Coming out of ESC, we'll have data in, I think, 16,000 patients.” It’s time, he said, for the US Centers for Medicare and Medicaid services in the US “to pay attention to this overwhelming level of evidence.”
Others speaking in this session or in the corridors afterwards were less convinced, particularly by the notion that IVI should have a role in all coronary procedures.
“I would say that for OCT, we were waiting for astonishing evidence showing a reduction in big events and this didn't happen,” Davide Capodanno, MD, PhD (University of Catania, Italy), told TCTMD, adding that it may be too much to ask of these tools. That said, he continued, “there are situations where you want to see what you are doing, and angiography is really imperfect in that respect.”
ILUMIEN IV and OCTOBER
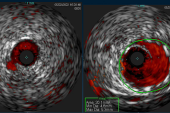
The first study to take the spotlight today was one of the most hotly anticipated trials in this space. ILUMIEN IV compared OCT with angiography to guide PCI in nearly 2,500 high-risk patients with high-risk lesions, and it demonstrated better stent placement with OCT on a range of metrics, including the primary imaging endpoint of final post-PCI mean stent area (5.72 mm vs 5.3 mm). OCT-guided PCI also led to statistically fewer stent thromboses (0.5% vs 1.4%; HR 0.36; 95% CI 0.14-0.91) and fewer procedural complications, but there was no difference in rates of the primary clinical endpoint of target lesion failure at 2 years (7.4% vs 8.2%; HR 0.90; 95% CI: 0.67-1.19).
OCTOBER, on the other hand, comparing OCT to angiographic guidance in complex bifurcation lesions in 1,200 patients, showed that the former significantly reduced the risk of MACE at 2 years (10.1% vs 14.1%; HR 0.70; 95% CI 0.50-0.98). A range of secondary endpoints, including a patient-centered composite of all-cause mortality, cardiac death, and target-lesion MI, all numerically favored OCT-guided procedures, but none met statistical significance. Rates of stent thrombosis were 2.1% in the OCT-guided procedures and 3.0% in the angiography-guided group (HR 0.70; 95% CI 0.34–1.47).
The disparate outcomes from ILUMIEN IV, presented by Ziad Ali, MD, DPhil (St. Francis Heart Center, New York Institute of Technology, NY), and OCTOBER, presented by study coordinator Lene Nyhus Andreasen, MD (Aarhus University, Denmark), produced palpably different reactions in the crowd that turned out for the intravascular imaging Hot Line. OCTOBER produced murmurs of approval, while ILUMIEN IV was met with something akin to surprised silence. Many interventionalists, on the basis of ILUMIEN III and prior meta-analyses, had assumed that statistical power was likely all that was needed for OCT to show an impact on both mean stent area and clinical outcomes.
ILUMIEN IV was “a big, big surprise,” OCTOBER lead investigator Niels Ramsing Holm, MD (Aarhus University, Denmark), who presented the results to the press yesterday, told TCTMD, particularly since ILUMIEN IV was such a “very well-done, well-performed study.”
But Holm wasn’t the only one left scratching his head. Deepak Bhatt, MD, MPH (Icahn School of Medicine at Mount Sinai), one of the Hot Line moderators, posed the question to Ali, ILUMIEN IV’s principal investigator: “What would you say to the purists who say: the trial didn’t actually meet its primary endpoint and everything else is just hypothesis-generating?”
Ali replied: “I think the finding of stent thrombosis is extremely meaningful, and I think it's meaningful because OCT does what it says on the box. It lets you look inside the artery, lets you identify the tissue protrusion, malapposition, dissections, and untreated reference segment disease, which biologically are directly applicable to the possibility of stent thrombosis.”
I'm definitely disappointed, but I'm a scientist and after disappointment comes analysis. Ziad Ali
Ali, speaking with TCTMD, said, “I'm definitely disappointed, but I'm a scientist and after disappointment comes analysis.” What ILUMIEN IV makes clear, he said, is that stent optimization is superior with OCT as compared with angiographic guidance, and complications are statistically fewer. Better stent sizing and deployment didn’t translate into significant reductions in target lesion failure here, but he suggested there are a number of possible explanations.
For one, operators are getting consistently better at placing bigger stents, even with standard angiography. As well, he speculated, the trial was conducted during the COVID-19 pandemic, when hospital avoidance and fear of contagion likely had an important impact on repeat revascularizations in particular.
While ILUMIEN IV failed to deliver the answer on clinical endpoints, the significant difference in intraprocedural complications and the “very strong 74% reduction in stent thrombosis is a big deal,” he said. “When I have to discharge a patient, what they want to know is, am I going to drop dead in Costco? Not: am I going to have some recurrent chest pain and going to have to come back to the hospital? So this is very meaningful to patients. And overall, I think with the totality of evidence, especially with the meta-analysis, there's really strong evidence that this works.”
ILUMIEN IV and OCTOBER were published simultaneously in the New England Journal of Medicine.
Looking for Meta-analysis Answers
Less controversially, the third trial in the session, OCTIVUS, which was published in Circulation and compared OCT to IVUS, established that the former is noninferior to the latter for guiding PCI. “In real world practice, still, the main [choice] of cardiologists predominantly is IVUS,” presenter Duk-Woo Park, MD, PhD (Asan Medical Center, Seoul, South Korea), told TCTMD. “These trials demonstrate that if you have some experience of IVUS or OCT, you can choose either one.”
That left the fourth Hot Line presentation, by Stone, to try to settle any controversy prompted by the seemly contradictory results of the two OCT versus angio trials. This updated meta-analysis combined OCTOBER and ILUMIEN IV along with others for a total of 20 randomized trials, all comparing some form of IVI-guided PCI with standard angiography guidance in 12,428 patients with chronic CAD or acute coronary syndromes.
Of the more than 7,000 in the IVI arm, 3,120 were randomized to IVUS and 2,826 to OCT guidance, and an additional 1,092 randomized to the operator’s choice of either modality (thus needing to be analyzed separately). In all, 5,390 patients were randomized to angiographic guidance.
In this large, pooled analysis, with patients having a range of different complex patient- and lesion-specific characteristics, the primary endpoint of target lesion failure (cardiac death, target-vessel myocardial infarction, or target-lesion revascularization) was a relative 31% lower in the IVUS/OCT group than in the angiography group. Moreover, cardiac deaths were reduced by 46%, target-vessel MIs by 20%, target-lesion revascularizations by 29%, and stent thrombosis cases by more than 50%—all statistically significant differences.
Of note, when analyzed separately, outcomes for OCT-guided procedures were very similar to those of the IVUS-guided procedures, as compared with angiography, and similar to each other, Stone said.
Worth noting, he stressed, is that while the reductions in cardiac mortality and MI did not reach statistical significance in ILUMIEN IV, for which Stone was study chairman, they were of the same magnitude as those seen in the meta-analysis.
Stone’s conclusion: “The routine use of OCT or IVUS to guide most PCI procedures will substantially improve patient event-free survival, enhancing both the long-term safety and effectiveness of the procedure.”
“Hopefully, this will impact the guidelines,” Stone told the press. “And if it gets a class 1 recommendation in the guidelines, that will make a difference, but we also need to work on removing the impediments to increasing intravascular imaging guidance for most patients in PCI.”
That’s not just a question of reimbursement, said Stone, but also training. “We have to train our attendings better [and] the attendings have to train the fellows better. It just needs to become part of the procedure.”
There are situations where you want to see what you are doing, and angiography is really imperfect in that respect. Davide Capodanno
Speaking with TCTMD, Capodanno, who was the discussant following Stone’s presentation, noted that the evidence in support of intravascular imaging is already “solid.”
“No matter which [tool] you select versus angiography, it will win,” he said. That’s based on evidence directly comparing the strategies, most of which compared IVUS with angiography. “The novelty today was the OCT versus angio [from] two conflicting trials, which are OCTOBER and ILUMIEN IV. And overall, the feeling is that the network meta-analysis shows a benefit, but this benefit is indirect, it's not due to the direct evidence, which was pretty neutral, so this is where I would be very cautious.”
Ideally, he added, another large, adequately powered trial directly comparing OCT to angiography would show a benefit on clinical events, but that should not take away from the fact that both OCT and IVUS are likely complementary and, taken together, are better than angiography in complex procedures. Like Stone and Ali, Capodanno pointed to cost and reimbursement as factors in underuse, but agreed that the largest barrier is training and confidence—particularly with OCT—in interpreting and applying the imaging results.
Enough to Change Practice?
Following the four Hot Line presentations, Bhatt polled the audience as to whether the evidence they’d just seen was persuasive enough to warrant a guideline change: in his estimation of the show of hands, a “majority” voted yes. Roughly the same proportion said they believed use of IVI likely is associated with a mortality reduction.
Asked which modality they would use, audience voters seemed equally distributed between IVUS and OCT users. Lastly, in response to a final poll by Bhatt, roughly half of voting audience members said they believed intravascular imaging should be used in all coronary procedures, while a similar proportion said it should be reserved for complex procedures and patients.
Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai), speaking with TCTMD, said she will need more evidence before shifting her practice on the basis of ILUMIEN IV. “I obviously was disappointed not to see a relationship between the stent expansion, which was better with OCT, [and] target vessel failure, but we have to accept that this is a negative result. In this patient population, using OCT, with a well-powered study, did not improve target vessel failure,” she said. “There was a signal of [reduced] stent thrombosis, but that needs to be further evaluated, because they were underpowered to say anything important about stent thrombosis.”
Intravascular imaging should be incorporated into your practice, but how you do it, and who you do it in is important. Roxana Mehran
Picking up on a point also made by ILUMIEN IV discussant Hector Garcia-Garcia, MD, PhD (Medstar Washington Hospital Centre, DC), in his review of the trial, Mehran dismissed the idea that the COVID-19 pandemic affected the trial outcome, because another IVI trial, RENOVATE-COMPLEX PCI, was performed over the exact same period and didn’t see an impact from pandemic lockdowns.
“What I think this tells us is that intravascular imaging should be incorporated into your practice, but how you do it, and who you do it in is important,” Mehran said.
So, even after four studies afforded 90 minutes in the limelight at ESC 2023, pinning down what patient or lesion characteristics would identify a procedure best suited to intravascular imaging remains elusive, even if all of the experts who took to the stage agreed: everyone performing PCI procedures should be using it more than they do now.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Kang D-Y, Ahn J-M, Yun S-C, et al. Optical coherence tomography-guided or intravascular ultrasound guided percutaneous coronary intervention: the OCTIVUS randomized clinical trial. Circulation. 2023;Epub ahead of print.
Holm NR, Andreasen LN, Neghabat O, et al. OCT or angiography guidance for PCI in complex bifurcation lesions. N Engl J Med. 2023;Epub ahead of print.
Ali ZA, Landmesser U, Maehara A, et al. Optical coherence tomography–guided versus angiography-guided PCI. N Engl J Med. 2023;Epub ahead of print.
Stone GW. Intravascular imaging guidance for PCI: a “real-time” updated network meta-analysis. Presented at: ESC 2023. August 27, 2023. Amsterdam, the Netherlands.
Disclosures
- Ali reports receiving research contracts from Abiomed, Abbott, Acist, Boston Scientific, Chiesi, HeartFlow, Medtronic, Nipro, Opsens, Philips, Shockwave, and Siemens, and consulting/royalties/owner/ stockholder payments from Philips, Shockwave, and AstraZeneca.
- Park reports research grants or speaker’s fees from Abbott Vascular, Medtronic, Daiichi-Sankyo, grants from ChongKunDang Pharm, and grants from Daewoong Pharm.
- Stone reports research grants with Abbott, Abiomed, Bioventrix, Cardiovascular Systems Inc, Phillips, Biosense-Webster, Shockwave, Vascular Dynamics, Pulnovo, V-wave; consulting/royalties/owner stockholder of Abbott, Daiichi Sankyo, Ablative Solutions, Robocath, Miracor, Vectorious, Valfix, Therox, HeartFlow, Neovasc, Ancora, Elucid Bio, Occlutech, Impulse Dyanmics, Adona Medical, Millenia Biopharma, Oxitope, Cardiac Success, HighLife, Cagent, Applied Therapeutics, Biostar family of funds, SpectraWave, Orchestra Biomed, Aria, and Xenter; and speakers’ honoraria from Medtronic, Abiomed, and Boehringer Ingelheim.
- Andreasen reports no relevant conflicts of interest.
- Both ILUMIEN IV and OCTOBER were funded by Abbott, and others.




Comments