IVUS in Complex PCI Improves Outcomes, Even for Less-Experienced Operators
Regardless of how many years an operator has done PCI, with IVUS the 10-year risk of cardiac death/target-vessel MI is lower.
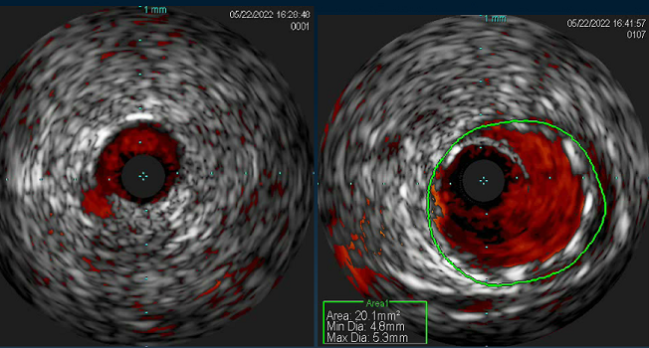
Photo Credit: Adapted from Mishra P. IVUS saves the day! Presented at: TCT 2022. Boston, MA.
For PCI in complex lesions, both the operator’s lifetime experience and the use of IVUS to guide the procedure appear to positively impact patients 10 years down the line, with less cardiac death and target-vessel MI, according to Korean registry data. In fact, the benefit that IVUS added over angiography was more pronounced when operators had less than 5 years’ experience.
Joo-Yong Hahn, MD, PhD (Samsung Medical Center, Seoul, Republic of Korea), senior author of the study, told TCTMD that its results offered some surprises.
“First, compared with less-experienced operators, experienced operators used IVUS more frequently, which was the opposite of what we had expected,” he said in an email. “Second, patients treated by less-experienced operators showed a comparable long-term risk of cardiac death or target-vessel MI to those treated by experienced operators when IVUS was used during complex PCI.”
Back in March, their group reported results from the RENOVATE-COMPLEX-PCI trial showing that complex PCI procedures guided by intravascular imaging—either IVUS or optical coherence tomography (OCT)—resulted in less target-vessel failure than those informed by angiography. “The present study using real-world data,” said Hahn, “further supports the benefits of IVUS.”
The new findings were published in the July 24, 2023, issue of JACC: Cardiovascular Interventions.
John W. Hirshfeld Jr, MD, and Michela Faggioni, MD (University of Pennsylvania, Philadelphia), in an accompanying editorial, say the study comes from a unique vantage point. “Despite being a single-center registry, their dataset is remarkable for its size, duration of case acquisition, data element granularity, and follow-up completeness,” they note.
Overall, these results suggest “IVUS guidance can partially offset the detriment of inexperience,” Hirshfeld and Faggioni say.
Alexander G. Truesdell, MD (Inova Heart and Vascular Institute, Falls Church, VA), who led the American College of Cardiology Interventional Council’s state-of-the-art review advocating for intravascular imaging in PCI that came out earlier this year, said the new analysis reinforces what’s been a consistent message.
“Every single study points the same direction: that there are hard outcomes benefits for an increasing number of lesion types with use of intravascular imaging in PCI. That story is only headed in one direction,” he commented to TCTMD.
Every single study points the same direction: that there are hard outcomes benefits for an increasing number of lesion types with use of intravascular imaging in PCI. Alexander G. Truesdell
Led by Ki Hong Choi, MD, PhD (Samsung Medical Center), the researchers looked at 6,005 patients (mean age 63 years; 75% male) who received drug-eluting stents for complex lesions at their center between March 2003 and December 2015.
Experienced operators—those who had lifetime independent experience with coronary revascularization > 5 years at the time of the procedure—performed the PCI in 63.4% of the patients, while the remaining 36.6% were treated by a less-experienced operator. Annual PCI volumes were higher for more-experienced operators compared with those with less experience (mean 255.6 versus 227.2 cases). They also more often used IVUS during complex PCI (29.6% vs 24.8%; P < 0.001 for both).
Median follow-up was 64 months. Risk of cardiac death or target-vessel MI, the study’s primary endpoint, was lower at 10 years for patients treated by operators with at least 5 years of experience (adjusted HR 0.779; 95% CI 0.663-0.915), with added benefit seen for every 1 year of experience beyond that threshold (HR 0.968; 95% CI 0.952-0.985).
Regardless of operator experience, patients whose PCI was done under IVUS guidance had a lower 10-year risk of the primary endpoint—the risk reduction was greatest when IVUS was used by less-experienced operators (P for interaction = 0.037).
Ten-Year Risk of Cardiac Death or Target-Vessel MI
|
|
With IVUS |
Angiography Alone |
Adjusted HR (95% CI) |
|
More Experience |
13.5% |
18.0% |
0.747 (0.559-0.998) |
|
Less Experience |
11.4% |
23.5% |
0.477 (0.337-0.673) |
Independent predictors of lower risk included not only experience and IVUS use but also transradial access. Age, diabetes, chronic kidney disease, ACS, LVEF < 40% on echocardiography, history of MI, multivessel disease, and left main CAD all independently predicted higher risk.
The US Lags Behind
The editorialists point out that a salient detail in this study is that operators, regardless of whether they were categorized as having low or high experience, had procedural volumes that far exceed the minimum of 50 cases per year set by US professional societies as the threshold for maintaining competency. Yet, as reported by TCTMD, many operators in the United States fail to meet this bar.
Uptake of intravascular imaging in the United States has also lagged behind the evidence. A paper published earlier this month in the European Heart Journal shows that even though use of IVUS or OCT during PCI rose among Medicare patients from 2013 to 2019, it only reached 15.4% by the study period’s end. That was for all cases, not just those involving complex lesions.
For complex PCI, IVUS use in Korea has now risen above 50%, Hahn confirmed, although usage by some operators remains patchy. “Medical cost is the most important hurdle. Additional efforts and procedural time may also explain operators' reluctance to use IVUS.”
Hahn urged systemic education programs, so that junior operators can become more comfortable with intravascular imaging early in their careers.
In the US, write Hirshfeld and Faggioni, a mix of factors such as “operator knowledge, financial concerns (an IVUS catheter costs approximately $725), and longer procedural times are likely the most common barriers” explaining the slow, heterogeneous uptake of IVUS. “As a result of spotty intravascular imaging use, interventional cardiology training in this important skill set is also variable among training programs,” they observe.
Operators should more consistently incorporate IVUS into their procedures, and training programs should be more robust, the editorialists say. Moreover, “Currently practicing interventional cardiologists who have limited IVUS knowledge/experience should seek mentoring relationships with more-experienced operators and strive to become proficient with intravascular imaging.”
Truesdell agreed that the Samsung Medical Center operators, by virtue of their annual volume, were all quite experienced. It will take a concerted effort at the individual, hospital, and professional society levels to train lower-volume operators in the US, he said.
With the existing data and what’s soon to come from clinical trials, however, he expects intravascular imaging to become a class 1 indication in US guidelines. The strongest evidence for IVUS use is in complex lesions: left main disease, chronic total occlusions, or lesions that are in-stent, long, or calcified. “But that’s already a very significant subset of the lesions that we’re facing,” said Truesdell, adding that it’s not that far of a leap to envision routine use in more-straightforward cases.
Ongoing trials in this space include ILUMIEN IV, OCTOBER, and OCTIVUS, results for which are scheduled to be released in a hot line session at the upcoming European Society of Cardiology meeting in Amsterdam. Others include IMPROVE, IVUS-CHIP, OPTIMAL, and DKCRUSH VIII.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Choi KH, Lee SY, Song YB, et al. Prognostic impact of operator experience and IVUS guidance on long-term clinical outcomes after complex PCI. J Am Coll Cardiol Intv. 2023;16:1746-1758.
Hirshfeld JW Jr, Faggioni M. Optimizing coronary interventional procedure outcomes: experience matters, intravascular ultrasound helps._ J Am Coll Cardiol Intv_. 2023;16:1759-1762.
Disclosures
- Choi, Hahn, Hirshfeld, and Faggioni report no relevant conflicts of interest.
- Truesdell reports having served as a consultant for/on the speakers’ bureau of Abiomed and Shockwave Medical.



Comments